Blog
Common Eyelid problems related to dry eye disease, Part 5: Floppy Eyelids!
When eyelids turn in the wrong direction: Floppy lids, malocclusion and snoring – a bad combination.
How can snoring be related to dry eye? - As a dry eye specialist, I can say there is a common connection. It turns out that the elastin (the tissue that gives the "elastic snap") to your voice box/airway area is the same type of elastin that is in your eyelids. If that elastin is weak, then lids lose their "snap" and can stretch out - making the lids tend to lose contact with each other when you relax (as in sleep) and they can pull away with gravity, exposing your eyes to room air (or to the ""blow-by" from a CPAP machine). Fans, Air Conditioning, or the rush of air from CPAP, (CPAP stands for Continuous Positive Airway Pressure, which is a machine that uses mild air pressure to keep breathing airways open while you sleep.) -
Image from: https://www.nhlbi.nih.gov/health/cpap illustrating (one of many options) CPAP device in use..
Image from: https://www.nhlbi.nih.gov/health/cpap
can cause increased evaporation of the tears that are exposed - and then your eyes get drier. When an eye doctor asks if you snore, they are trying to see if you might have Obstructive Sleep Apnea.
Below from the Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/sleep-apnea/symptoms-causes/syc-20377631
“Obstructive sleep apnea
Above taken from the Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/sleep-apnea/symptoms-causes/syc-20377631
“Enlarged image
Obstructive sleep apnea
This type of sleep apnea happens when the muscles in the back of the throat relax. These muscles support the soft palate, the triangular piece of tissue hanging from the soft palate called the uvula, the tonsils, the side walls of the throat and the tongue.
When the muscles relax, your airway narrows or closes as you breathe in. You can't get enough air, which can lower the oxygen level in your blood. Your brain senses that you can't breathe, and briefly wakes you so that you can reopen your airway. This awakening is usually so brief that you don't remember it.
You might snort, choke or gasp. This pattern can repeat itself 5 to 30 times or more each hour, all night. This makes it hard to reach the deep, restful phases of sleep.” Taken from the Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/sleep-apnea/symptoms-causes/syc-20377631
________________________________________________________________________________________________
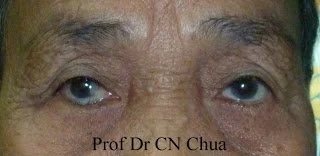
Having symptoms of drier eyes on waking can be related to loose or "Floppy" lids (as well as to sleeping with normal lids that don’t close all the way when sleeping – see my earlier post on “Mom’s eyes” in the link below). When eyelids are “too floppy” the eyelids can roll over, (or become an “outtie” – similar to the discussion on ectropion) or can “mal-occlude” – where they don’t come together well enough (and the upper lid may slide over the lower lid, creating a gap that doesn’t wet well and may result in the lashes irritating the underside of the upper lid). To determine if this may be the case, doctors need to look under the lids to test how “floppy” they are and to observe the moist membrane (conjunctiva) lining the lids (giving further clues about your eye condition).
If you snore (or suspect you snore - a spouse or significant other can help confirm it), and you are found to have floppy lids, then the "Floppy Eyelid Syndrome" seems likely related, and the doctor will commonly recommend you check with your Primary Care Physician about getting a "Sleep Study." During a sleep study, the staff will be looking for sleep apnea (described above - the condition where your airway blocks mid-snore, and you can go lengths of time not breathing). Sleep apnea has been linked to early death (heart attacks, strokes, etc.) and may contribute to ever-weakening elastin - making dry eyes worse and your life in general - quite miserable - if not shorter than it would otherwise be. Get a sleep study if your doctor recommends it (and wear the devices prescribed - like CPAP, as they can save your life). Sleep goggles, Press N Seal or Sleep Tite Sleep Rite adhesive stickers can help, as can humidifying the air in your CPAP machine, humidifying your room air and making more and better tears as I outline in earlier posts (like the “Mom’s or Dad’s eyes” post here: https://www.eyethera.com/blog/do-you-have-moms-or-dads-eyes
When lids are too “Floppy,” surgical tightening is sometimes indicated, though the above recommendations are frequently sufficient to “work-around” the problem.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Common eyelid problems related to dry eye disease, Part 4: The eyelid “innie.”
Right Lower Eyelid is turning/rolling inward and putting the lashes against the white part of the eye, courtesy: eyewiki.AAO.ORG.
Part 4: When eyelids turn in the wrong direction: Entropion = turns in
https://eyewiki.aao.org/Entropion
Right Lower Eyelid is turning/rolling inward (entropion) - and putting the lashes against the white part of the eye (trichiasis).
Entropion (or inward turning lids) will result in the lashes rubbing on the conjunctival and/or corneal surfaces (called trichiasis), so that the surface can become scratched and irritated. This can be more destructive than when the lid turns out, in that continuous rubbing of lashes is a bit like adding a hairbrush to the blink. This accelerates making normally smooth conjunctival membranes red and rough, but when directed against the delicate cornea (the clear “window” of the eye) this “hairbrush” called trichiasis, can cause stronger irritations and larger, more painful scratches/abrasions. Adding the mix of germs that like to live along the base of eyelashes and the lid margin into those “open sores” is a potential recipe for disaster. As is also true for ectropion, corneas do not feel good, nor do they see well when they are dry, rough or continually scratched but can go bad in a hurry when infected.
To fix an Entropion, it is important to determine the cause, and surgery may often be required. Like ectropion, not excessively rubbing the eyes helps avoid the stretching and weakening of the ligaments that support the lid in its normal position. Weak ligaments allow the “hammock” to tip - in this case, inward. If the cause is “floppiness” (see my upcoming post on floppy eyelids and related sleep apnea), then dealing with the sleep apnea can often help stop further floppiness and may help repair it over time. When there is entropion-related lash rubbing/scratching (trichiasis), then it is common to have reflex tearing, where the “fire hose” turns on and salty water floods the eye. This is less helpful, as the salt will sting the corneal sores caused by the scratching and salt water provides little lubrication. This can break down the surface quickly and can readily lead to infections, scarring and loss of vision.
Trachoma and related eye and eyelid disease
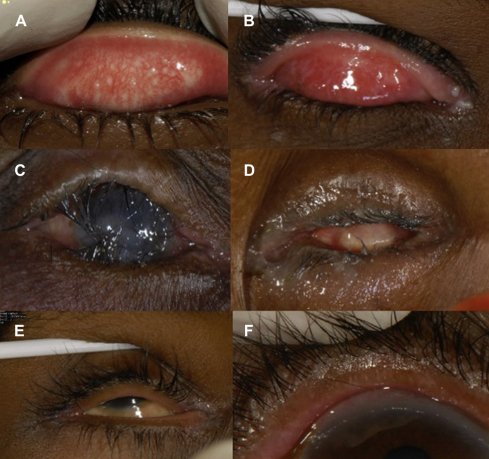
The clinical signs of trachoma. A: Active trachoma with both follicles and intense inflammation. B: Trachomatous conjunctival scarring. C: Entropion trichiasis and corneal opacity. D: Phthisis. E: Misdirected lashes. F: Metaplastic lashes. Surv Ophthalmol. 2012 Mar; 57-341(2): 105–135.
While rare in the USA, trachoma is still the leading cause of blindness in less developed countries - and will commonly lead to the inturning of the lids - with lid, and then corneal scarring. Fortunately, if caught early, it is easily treatable with the right antibiotics and preventable with good hygiene, as it is caused by a germ that is easily spread by personal contact and is therefore very contagious. Prior surgeries, injuries (especially chemical injuries) and chronic inflammation from infections (apart from trachoma) like blepharitis (see my earlier posts on this), or allergies, can also lead to degrees of this condition. Rare immune issues like Stevens-Johnson or Ocular Cicatricial Pemphigoid, as well as some persons born with this problem, also occur.
I should mention that lashes can turn in (trichiasis) without any inturning of the lid (entropion). These misdirected lashes can have a similar effect on the surface of the eye, but most often can be managed with selective removal of these lashes (see my earlier post on this here: https://www.eyethera.com/blog/0r1w3kiho48uaz4yydxlyrogx5xksf).
Having plenty of oil and healthful tears will help to lubricate and limit the scratching and help in repairing the roughened surfaces. However, it is hard to have the good blinks eyes need, when the lashes are rubbing with each blink. Better blinking would be beneficial to making those “good tears” but is hard to do until the lid position and “blink mechanics” are restored – so fixing the lid is often required to allow proper tear production and distribution.
When entropion is related to lid spasms (as can occur after any surgery on the eye), then a temporizing injection of Botox-like medication can quell the spasming until the eye is healed and the condition may not need much more treatment. Short-term “fixes” can be as simple as adding a piece of sticky tape that splints the loose lid, or pulls the lid out and away from the eye. A mild-to-moderate, in-office treatment can sometimes be offered using special dissolvable stitches to turn the lid outward, away from the eye (called Quickert sutures). This will create a certain amount of scarring and healing that can redirect the lid forces away from the eye, but will typically wear off over time. If an entropion is severe or progresses, then more surgery is generally required and may involve tightening the lid by surgically shortening it and then resuspending it to the natural “hammock attachment sites.” Surgically “re-draping” the muscles can help rebalance the “hammock,” when just re-suspending it, isn’t enough.
Many eyelid problems will be slower to occur if the eyelids get proper support and good care over one’s lifetime. Particularly, use of toxin-containing makeup materials, or, unchecked - the overgrowth of skin germs or environmental allergies, excess eyelid rubbing or stretching - these all add up to trouble and may result in this unwanted, unhealthy eyelid (and ocular surface) condition. Getting regular eye checkups and proper eye (and eyelid) care is essential to good eye health!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Common Eyelid problems related to dry eye disease, Part 3: The eyelid “outtie.”
Part 3: When eyelids turn in the wrong direction: Ectropion = turns out
Eyelids are critical to the wellbeing of the eye, as they provide the “heartbeat” that circulates the tears over the living surface of the eye, as well as protecting and supporting the eye in its socket. They are made of a tough “skeleton” (called the tarsus, or tarsal plate), with an inner lining of conjunctiva (the smooth, moist membrane that also covers the white part of the eye) and an outer layer of muscles and skin. There are tough ligaments that connect the lids to the eye socket bones at the inner and outer corners – and suspend the lids a bit like a “hammock.” Normally, the muscles controlling and supporting the lid activities of a blink, also help to “balance” that “hammock,” so it stays upright and in good alignment with the eyeball. Unfortunately, age, injury, surgeries, sun, tumors, nerve and muscle weaknesses and genetics can all contribute to an “imbalance” of the muscles, resulting in a “tipping” or turning of the “hammock.” This can lead to an outward turning (Ectropion) or inward turning (Entropion) – and each has expected (and sometimes unexpected) consequences. Below is an example of ectropion:
Involutional ectropion of the left lower eyelid. Keratinization of the palpebral conjunctiva is present. Image courtesy of Marcus M. Marcet, MD FACS. https://eyewiki.aao.org/Ectropion#:~:text=There%20are%20four%20main%20types,cicatricial%2C%20mechanical%2C%20and%20paralytic.
Ectropion (or the outward turning) of an eyelid will result in the pink, conjunctival surfaces becoming exposed to room air. This is a normally pink, moist membrane akin to the lining of your mouth. (Imagine how dry and awful your mouth could feel if you left it open all the time, so that the lining would become dry and irritated). That continuous exposure could also allow the normally moist eye membranes to become more like your skin and less like the thin, smooth, moist membrane that it should always be (this transformation to a skin-like surface is called keratinization). Skin is a rougher, drier covering – so that rough, skin-like surface could end up rubbing against the delicate cornea (the clear “window” of the eye). Corneas do not feel good, nor do they see well when they are continually scratched. The out-turning of the lid can also make it hard for the cornea to become refreshed with tears when you blink, as the tears may roll over the out-turned lid rather than be pumped up over the eye with a blink (more on this below).
To fix an Ectropion, it is important to determine the cause, and surgery may often be required. Avoiding sun damage is usually as simple as wearing sunglasses and using sunblock. Not excessively rubbing the eyes helps avoid the stretching and weakening of the ligaments. If the cause is “floppiness” (see my upcoming post on floppy eyelids and related sleep apnea), then dealing with the sleep apnea can often help stop further floppiness (and may help repair it over time).
When there is ectropion-related exposure, then having plenty of healthful tears will help to limit the dryness, exposure and scratching that is otherwise common. However, it is hard to have the good blinks which are beneficial to making good tears until the lid position and “blink mechanics” are restored – so fixing the lid is often required to allow proper tear production and distribution. Caught early, a small operation like “ignipuncture” (tiny burns applied in a precise way) can help support and turn the lid back to a normal position with the tightening from healing, caused by this procedure. In-office treatments can be offered using radio frequency technology, for that purpose. If an ectropion progresses, then more surgery is generally required and may involve tightening the lid by surgically shortening it - and then “resuspending it” to the natural “hammock attachment sites.” Surgically “re-draping” the muscles can help rebalance the “hammock,” when just re-suspending it isn’t enough.
Even a small out-turning of the inner corner of the eyelid can present a problem, as it can put the opening to the tear duct beyond the pool of old tears that would usually be drawn into the tear duct with a blink. This normal event is what allows proper turnover of the tears on the eye (remember the old, dirty, used-up tear has to be replaced by the fresh, healthy tear every time you blink. The old tear goes down the tear duct and ends up in the back part of the nose - but only if it can find its way to the opening of that tear duct. The “windshield wiper” function of the lid is also what brings the healthy tears up to replace the old tears - and a turned out lid can ruin the “wiper” function and interfere with even that level of proper “circulation.”)
The opening to the tear duct is called the punctum and once it drifts away from the eye, we call it a “punctal ectropion” and the effect can cause tears to bypass the normal tear duct and track down the inner corner of the lid. This will cause tears to run down the cheek, making it look like you’re emotionally crying. This type of tearing can also occur from blockages within the tear duct system, from loose or excess conjunctival membranes blocking the surface of the tear duct or acting as a “water slide,” diverting tears (from conjunctivochalasis - see my earlier postings on this, beginning here: https://www.eyethera.com/blog/what-is-conjunctival-chalasis-cch-and-why-should-i-care ) or from excessive “reflex tearing” caused by excessive dryness (see my post on overly salty tears and “reflex tearing” here: https://www.eyethera.com/blog/overly-salty-tears ) - so your doctor should check to find the cause of abnormal tearing and then treat it accordingly.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Common eyelid problems that can relate to dry eye disease, Part 2: Say Hi to “TED.”
TED is not this patient’s real name but the acronym as described below. The rights to this photo belong to the company making the treatments described below and in this link: Tepezza
Exposure from eyelid retraction– “The Thyroid Stare” (Exposure from: Thyroid Eye Disease=TED, related to the higher levels of thyroid hormone) and/or proptosis from thyroid-related inflammation (among other inflammatory causes) behind the eye, causing eyeball “bulging.” Some unfortunate patients may have a combination, causing a high degree of eye exposure (as in the top photo before treatment, above - vs the lower above photo, after treatment) – resulting in dry eyes even when tears are otherwise good (but especially bad if the tears are “bad”). Untreated, in some cases this can lead to permanent loss of vision.
Conditions where inflammation gets behind the eye can cause the eye to be “pushed forward” - a condition called proptosis or exophthalmos, it results in the eye bulging out of the natural protection of the “bony cave” of the skull (the “orbit”) – to where the surface is exposed more than normal. This is common in Thyroid-related eye disease (TED), but can be found in other cases of genetically “shallow” orbits, inflammation, infection or from tumorous growths behind the eye(s).
If someone has TED (or any other reason for an over-exposed eyeball), then there are standard, and then newer treatments available, depending upon the degree of involvement and how much damage exists - or is at risk to exist. Job number one is to make great tears – since great tears can take good care of even very exposed eyes and bad tears can be especially bad for these eyes.
The clinical goal is to keep eyes safe and comfortable – but this can sometimes sacrifice form over function. By this, I mean that surgeries can be done to pull lids partially together (a so-called lateral and sometimes medial tarsorrhaphy) or to put a spacer into the lid to let it drop down to cover the eye better, but this may not look as cosmetically pleasing as if the eye were just to “look normal.”
This image is an example of a lateral tarsorrhaphy taken from the archives of the American Academy of Ophthalmology AAO photo and shows how the lids are brought closer together to partially cover an otherwise overly exposed eye. The cloudy, raised spot over the pupil is a corneal scar caused by excess exposure and can reduce vision in ways that is difficult to repair.
“Standard” therapy begins with all the “usual” homework for dry eye (see my earlier posts on this) and efforts to produce more and better tears as eyes bulge and exposure worsens. Adding lubricants, Autologous Serum Tears, sleep goggles and ointments at nighttime, and anti-evaporative wraparound glasses by day - can be increasingly helpful, as is true for most advanced dry eye patients. Monitoring how the inflammation and congestion behind the eye is affecting the eye-movement muscles, and the nerves involved with sensation - and particularly with vision – is key to maintaining eye health. If the eye’s health becomes compromised (double vision, pressure on the nerves, over-exposure of the eyes), then increasing levels of intervention are often required.
The common advanced interventions included steroids (prednisone) to reduce inflammation, radiation (when steroids prove insufficient or poorly tolerated) and surgeries (to decompress the swelling behind the eyes) – where bone and inflammatory tissues are removed to “make room” behind the eyes - as required to preserve eye health and function. Inflamed muscles will swell and cause poor function, resulting in double vision. Too much swelling can “pinch” the nerves, causing pain and permanent loss of vision, or cause over-exposure, causing damage to the surface of the eyes. Eventually the inflammation tends to “burn out” – so conventional wisdom was to address swelling with enough treatments to buy enough time for the inflammation to eventually subside. Smoking tobacco is like adding gas to the fire of inflammation and is strongly discouraged.
Fortunately, Tepezza is a new medication used as an infusion to fight the source of the inflammation unique to TED and has proven extremely effective against the swelling and related damage. Like most strong medications used to treat bad diseases, it can have a host of side effects that need to be weighed against the risks of the disease it is treating. These are generally manageable, but can include permanent, irreversible hearing loss in some, so proper monitoring of progress is equally important and choosing this treatment is best left to experts in the field. Dry eye doctors can help support the health of the surface of the eyes by promoting great tears and assisting in the monitoring of surface health if the disease progresses.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Common eyelid problems that can relate to dry eye disease, Part 1: Bad lashes.
Trichiasis (lashes rubbing on the eye = “Bad Lashes”):
Many of us have had to pull an errant eyelash out of our eye or eyelid at some point. If the lash was totally loose and freely riding on the eye, then this is a common and “normal” occurrence, usually fixed by simple irrigation (either from tearing that washes it out, or by an eye wash rinse). But if the lash is still attached to the lid by its root, while rubbing on the eye, then this is an “abnormal” problem called trichiasis. This can be painful and in severe cases, lead to infections, scarring and loss of vision.
This condition can be a genetic, predetermined problem (often in rows of many such errant lashes) or can occur due to thinning and scarring of the lid (cicatricial), or from the more common cause relating to “Blepharitis” (see my earlier posts on this). Blepharitis can cause one or more lashes to “grow wrong” so that they turn in and rub against the eye. Sometimes just pulling the lash (epilation) and treating the blepharitis will “fix it.” Sometimes it will continue to come back the same way and need further treatment.
While treatment can vary, it is also true that the “root” (the growth “bulb”) can be quite persistent and hard to “kill.” The normal life cycle includes 3-phases of the lash, beginning with a growth phase (Anagen), a dwelling phase (Catagen) and a falling out phase (Telogen), where the lash will eventually fall out and then gradually regrow (approximately a 6 week-long cycle from start to stopping growth and then falling out). To remove a lash effectively and permanently, it is best to target it in the growth phase, when it is strongly connected to its “root.” Laser or IPL of the correct wavelength, electricity or RadioFrequency (RF) can be used to permanently “kill” a lash. Surgery can remove the lash(es) and freezing (cryosurgery) is a more destructive way to permanently remove them – though either can be extremely effective, both of these options tend to be the more painfully invasive.
Skin of color, or those with very blonde, red, white or lighter-gray lashes will generally not respond to light-related (laser or IPL) removal, as the dark skin can prevent light from penetrating deeply into the lid where the root is (essentially shielding the root from the light) and lighter colored lashes have so little “pigment” (the color of the lash) in the root, that the light doesn’t get absorbed in a way that effectively kills the root. When you have light skin and a dark lash, this can be a quick and simple treatment, with little discomfort. This is generally true for hair of all sorts, regardless of the location, and is the basic principle for all so-called “Laser Hair Removal.”
Electricity (as electrolysis) or RF (hyfurcation) are effective alternatives for permanent lash removal of any skin color and in any location. They are also most effective if done while the hair or lash is in the growth phase – or at least the dwelling phase – as once the hair or lash goes into the falling out phase, it disconnects from the root and it is often impossible to treat the root once it is “disconnected.” The principle of killing the root is common to every type of permanent hair removal and the 3-phases of hair growth accounts for the main reason it is often impossible to remove all hair/lashes with one single treatment. If the root is “missed” (due to the hair or lash being disconnected), then it will require a second (and sometimes more) attempt to permanently “remove” it. Because eyelids are sensitive and eyes are close behind the lids, it is common to have an eye doctor help you with this. In the case of electricity or RF, a small amount of numbing is common to help make the brief application of energy comfortable. An insulated “wire” is introduced alongside the lash and a brief application of current will create a burst of energy into the root. Once the lash root is sufficiently damaged, the lash becomes loose and is easily removed. If the root was effectively “killed,” then it won’t allow the lash to grow back.
Again, it may take a monthly series of such treatments to fully remove all the bad lashes, depending on which phase they are treated, how well they are treated and how many are yet to develop and become present to be treated. Uncontrolled blepharitis is also a common recipe for more to come along, so controlling blepharitis is good for the tear glands as well as for the lashes and general health of the lids, lashes, and the eye itself.
For more information on trichiasis, see also:
https://www.aao.org/eye-health/diseases/what-is-trichiasis.
https://www.reviewofophthalmology.com/article/the-annoying-lash-in-the-eye-a-review-of-trichiasis
What about Punctal Plugs (or - “Why not dam up those tears”)?
As a dry eye specialist, I often get asked about using punctal plugs for dry eye disease control. I find that the answer to that very good question is the common “it depends” - in that those with good-quality tears but poor-quantity can do well with plugs in general - but poor-quality tears generally do not.
“Punctal plugs” are anything that can block the flow of tears from reaching the usual destination involving normal, tiny openings along the inner portion of upper and lower lids, that carry tears through a drainage system that ends up in the back of the nose, leading to the back of the throat. They intentionally block this natural system, where the old, used-up tear on the surface of the eye can be blinked away and down the throat, while the new, fresh tear comes up from the little “tear gutter” (called the fornix, it is the reservoir behind the lower lid) to replace the used-up tear. If a blink is the “heartbeat” of the eye, then this turnover is the “circulatory system.”. Retaining more tear volume can work wonders for some and be problematic for others. These plugs come in many forms and sizes to accommodate the anatomic variety we see among our dry eye patients. This Mayo Clinic link provides a quick overview and diagram: https://www.mayoclinic.org/diseases-conditions/dry-eyes/multimedia/punctal-plugs/img-20007894#:~:text=One%20approach%20to%20treating%20dry,tears%20you%20may%20have%20added.
Once the common causes of inflammation have been dealt with (see my earlier posts on inflammation) - if ATD prevails, then plugs can be an eye saver (but should be periodically checked, with good lid hygiene and often replaced - to keep them from accumulating biofilm and the germs it carries – see below and my earlier posts on lid hygiene).
Treating patients, my first goal is to determine the root cause(s) of the patient’s dry eye disease. If primarily MGD (Meibomian Gland Dysfunction – where malfunctioning oil producing glands are causing dry eye disease – see my earlier posts on this), then plugs tend to be less helpful and may make things worse (more on this in a moment). ATD (Aqueous Tear Deficiency, where the “Sprinkler System” makes too little water) means the tear volume is too low (since most tear volume is made from water) and is a more common target for punctal plugging, which will retain more of that tear on the surface of the eye. Unfortunately, many dry eye patients have a mix of MGD and ATD. Poor oil will cause rapid evaporation and lead to “dry spots,” which often requires the “Fire Hose” glands to kick in, causing what we call “Reflex Tearing.” This flood leads to overflow, which can make tears run down the face even with the normal, full function of the tear drainage system. The overflow can get much worse when the system is blocked off by these plugs if reflex tearing continues after the plugs are put in.
A common cause of ATD is inflammation. If there’s a lot of inflammation, then plugs generally make it worse, as this is a “poor quality tear” that - thanks to plugging - doesn’t leave, and perpetuates the dry eye problem by leading to higher levels of inflammation. I’ve heard this referred to as “leaving the dirty bathwater in the tub and expecting it to make you clean.”
If most oil and inflammation issues are reasonably controlled and the tear volume is the remaining, primary problem, then plugs can be a great help. The types of plugging available boils down to:
- Exposed plastic (usually silicone-derived) plugs inserted directly into the “mouth” of the openings along the lid (called the punctum), which have a form of inverted umbrella design to ensure they stay in place as an anchor. The small, “contact lens-like cover” functions as an “end cap” that is visible microscopically, but rarely to the naked eye.
- “Permanent” plugs made from, small, tubular forms of plastic designed to swell inside the tiny tubes or channels that connect the punctum to the nose. These are inserted through the punctum and are carried along the channel until the swelling - or a bend in the channel - “catches” the plug and traps further flow. They are invisible but not always permanent, as they may wash through the drainage system before they “grab” and fix to the lining of the channel.
- “Temporary” plugs made from dissolvable materials designed to swell inside the tiny tubes or channels that connect the punctum to the nose. These are inserted through the punctum and are carried along the channel until the swelling - or a bend in the channel - “catches” the plug and traps further flow, but then gradually “dissolves” and re-establishes flow. The rate of dissolving is a function of the materials used to make these plugs and the amount of irritation they may cause, which can provoke faster dissolution and may lead to scarring within the channels. Like the “permanent” internal plugs, they are also invisible and can also wash through the drainage system before fixing to the wall of the channel.
- Cautery - a small burn over the mouth of the punctum, causing a scar to act as the plug. The lid is numbed before the heat is applied, so this is typically a near-painless procedure. Punctal cautery is a more “complete” plug, in that plastic plugs typically allow a little “wicking” of tears around the plug, so there can still be a little clearance.
Since tears are best when “fresh” and since plugs and cautery encourage degrees of stagnation, there are patients who get less complete benefits. Also, though tiny, exposed plugs are plastic and can be viewed as smaller “contact lenses.” That said, they, like contacts, can accumulate “plaque” (like the grunge that accumulates on teeth and acts as footing for more germs), so changing out plugs periodically (& doing good lid hygiene) is generally required. Reflex tearing is common in dry eye patients and once the plugs block drainage, the only route “out” is by evaporation, the wicking around a plug or over the lid crying, so if you puddle up in a dry wind, then consider this as a likely side effect. Seasonally the benefit of plugs depends - as those with allergies may suffer more by keeping allergens like pollen in - but drier weather like in air conditioning or winter, may be better “fits” for the plugs as dry air means more evaporative loss (as long as the occasional reflex tearing is not too great of a nuisance).
With exposed, plastic plugs, it is usually easy to remove them if problematic (not so easy if cauterized). Plugs retained along the internal channels may be forcibly flushed in a way that can propel them through the system and into the nose. Obviously, cautery means no plastic materials are involved (but also may mean more stagnation), so there’s nothing to fall out or change. Cautery should be regarded as “permanent,” although the scar will sometimes “heal open” or – in cases where the reflex tearing is problematic, may be able to be operated on to re-open (though that can be difficult or impossible in some cases). Rarely, exposed, plastic plugs can trigger scar formation that can cover over or expel the plugs and removal can be problematic, as older plugs can become more fragile and break off, leaving retained pieces inside the lower opening (which may then require a small operation to retrieve).
I've generally shied away from the dissolvable or disappearing plugs as it is hard to know when they are gone (either dissolved or having been swept away and down the tear duct into the nose or mouth). Sometimes these “internal” plugs will trap just enough stagnant tear within the channel as to provide a happy “culture medium” for germs to thrive in – and infections from these kinds of plugs can be hard to treat as this may lead to an internal abscess that then requires surgical drainage to fix.
Common dry eye treatments like lid cleaning, heated expressions and IPL are not overly likely to displace the average plug. If it falls out or dissolves, it can be easily replaced - so whether that happens from a Blephex, Lipiflow or other manipulation, I don't see that as too bad (other than cost) as it is not a bad idea to replace plugs every so often anyway (as I mentioned that they can become breeding grounds for bacteria or other grunge). As a provider of BlephEx, IPL and various heated expressions of MGD, I've not let plugs stop me from recommending that treatment if it is indicated. Fortunately, Punctal Plugs are usually covered by most insurance, are quick and generally painless to place, equally easy to remove (if exposed) and replace when indicated. Check with your dry eye specialist to see if they may be right for you.
What happens when you don’t have enough good oil and how do you fix it? (SLK, CCH and why blinking matters)…
While I’ve posted about blinks and the effect of blinking on making oil (links below), I recently was asked about SLK (and thereby CCH) – two structural eye problems which are the result of poor oil. BioTissue, among others, have dubbed this poor oil problem as “Mechanical Dry Eye” (or MDE), as friction is a driver (so a mechanical force). However, I think there is an equal contribution from the evaporation relating to lack of the “Saran Wrap-like” sealant effect of oil (so water evaporates from our tears, leaving a higher concentration of salt to cause more surface damage and leads to inflammation. Inflammation added to friction “unpeels” the glue and fibers that hold the conjunctival membrane to the underlying white of the eye (or sclera), allowing it to “come loose.” Further friction leads to more inflammation and the vicious cycle perpetuates dry eye and related surface eye diseases.
SLK (superior limbic keratoconjunctivitis) is essentially the same as CCH (conjunctivochalasis) - both are when the conjunctival membrane "comes loose" and develops pleats and folds that interfere with the proper eyelid “squeegee” of tear flow over the eye, as well as causing friction-related irritation. Instead of affecting the lower part of the eye like CCH, SLK affects the upper. Surprisingly it appears to be less common than CCH, possibly because the inflammatory tear products are in greater contact with the lower lid from gravity, possibly because our eyes more commonly track downwards rather than upwards – possibly due to the differences of the mechanical forces relating to the difference in the size and position of the upper vs lower lids -but the effect of friction and inflammation on the conjunctival membrane is the same. It also appears more common in Thyroid-related eye disease and Rheumatoid Arthritis, but then so is my perception of CCH, too.
An autograft (where a portion of conjunctiva harvested from another area and “transplanted” to cover the area exposed when the damaged conjunctiva is removed) - or the amnion surgery used by some in CCH repair (where a piece of amnion is glued or sutured over the exposed area) can work - but I found that radio frequency (RF) works great for both CCH and SLK - and offers the opportunity to do an (off label) RF-heated expression of the clogged MGs that appear common to causing both SLK and CCH. In the past, Silver Nitrate (on a wooden stick applicator) was also used to treat SLK - but it causes a chemical burn rather than an electrocautery or RF-plication "singe" - so I didn't find it better (as it seemed less predictable and doesn't fix the problem - obstructive MGD - causing the problem – SLK as we can with RF).
For more on CCH, see these earlier posts: https://www.eyethera.com/blog/what-is-conjunctival-chalasis-cch-and-why-should-i-care and for some embedded links to see how I actually do my treatments (and a study I published on the success of these treatments), see:
https://www.eyethera.com/blog/conjunctival-chalasis-cch-part-2-how-do-we-fix-it
Lastly:
https://www.eyethera.com/blog/cch-part-3-when-do-we-treat-cch-and-what-are-the-options
Early in my career, when I began to specialize more fully in all things related to dry eye disease, I had the good fortune to spend some time with a true giant in that specialty (Dr. Donald Korb – inventor of Lipiflow). Due to his influence, I became one of the first doctors to offer Lipiview and Lipiflow north of Boston (where Dr. Korb invented it). I gained a huge appreciation for the variety of blinks and blinkers (Lipiview was the first commercial technology to monitor blinks). My experience is that those with uniformly poor blinks tended to have worse MGD (dysfunction of the oil producing glands of the eyelids) and those fortunate few who had better blinks tended to have less MGD.
As a fellow partial blinker, I can relate to how confusing this is. I see it as a measure of higher IQ (since I have the same issue;) but I believe it boils down to the fact that nobody teaches us how to blink, so some (perhaps most) of us learn these “bad blinks.” As children we had perfect eyes and perfect tears - so we hardly had to blink. As we “grow up” we don’t do ourselves any favors by partial blinking. Digital devices add to partial blinking by staring and then stagnating oils. I’ve posted on some of this stuff here:
https://www.eyethera.com/.../how-important-is-oil-to-our... and
https://www.eyethera.com/.../why-do-my-oil-supplements...
Here, I offer some tips on how to remedy our “bad blink habits:”
and
https://www.eyethera.com/blog/avoiding-a-heart-attack-on-the-surface-of-your-eye
Probably the best way to deal with this issue is prevention through education. Helping our children develop good habits - working on better blinks, encouraging more time spent outside where natural stimulation from wind and sun can help promote good blink habits (and hopefully less time spent on digital devices - or at least following the 20/20/20 rule), good diet and exercise programs - and proper lid hygiene. Add to that regular eye checkups that can include monitoring the health of our tears and the surface of the eyes.
Some years ago, I had the good fortune to come across a European PhD candidate who was focused on these blink issues and he produced a useful website you can visit here:
https://www.blinkingmatters.com/
Sjogren’s Disease: Autoimmune dry eye Part 5
The key question asked of Sjogren’s researchers is – “what does the future look like for Sjogren’s patients?” Fortunately, there are new consortiums of research activities that appear to bode well for a good answer.
Is a consortium of private corporations and government institutions structured to help understand and accelerate treatments for certain autoimmune diseases (Rheumatoid Arthritis and Lupus in particular) that are related to Sjogren’s Disease in some subsets of patients. Founded in 2014, there has been a lot of activity which is slated to continue over at least the next 4 years.
From their website, we find this:
“AMP-AIM” is a next-level evolution of the AMP program. From their website:
https://fnih.org/our-programs/AMP/autoimmune-and-immune-mediated-diseases
“As a next step, AMP AIM is working to refine and extend the single-cell analysis of biopsy (e.g., synovium, kidney, skin, salivary glands) and blood samples to include additional diseases, including psoriasis/psoriatic arthritis and Sjögren’s disease.” Finally, Sjogren’s Disease is getting the much needed spotlight it deserves from a consortium of heavy hitters who are in a great position to figure it out and effectively treat it!!
Dr. Nancy McNamara is an optometrist working at UCSF who notes that the cornea has the most number of nerves per square inch of any portion of the human body, so it perhaps no surprise that it can “hurt” even when we can’t clinically find anything out of place using conventional examination methods (the so-called “pain without stain”). Lacritin is a naturally occurring compound found in tears, which has a profound impact on restoring corneal nerves and the surface cells lining the cornea (epithelial cells). Measuring the amount in tears can help to increase our ability to find Sjogren’s patients, as they commonly have very low values of this compound. Equally exciting is the likelihood of soon treating eyes with extracts of this compound - a product called “Lacripep” (which is a smaller, active ingredient in Lacritin). Of a side interest to me, the company making this product is based in Charlottesville, VA (my Ophthalmology Residency alma mater). A recent study can be found here: https://journals.lww.com/corneajrnl/Fulltext/9900/Lacripep_for_the_Treatment_of_Primary.84.aspx
Dr. Anat Galor is an Ophthalmologist working out of the University of Miami, Bascom Palmer Eye Institute. She headed a small study looking into fecal microbial transfer from healthy donors to the gut of active Sjogren’s patients. Unfortunately, these transfers did not “take” long enough to have a significant impact on the receiving patient’s gut to show significant benefits, but there was enough promising data to turn attention towards a “customized biome transfer,” where needy patients could have pills tailored to the more precise germs required to “fix” their gut-related autoimmunity issues. She also pointed to the promising research using natural anti-autoimmune injections of intravenous immunoglobulins (IVIG) to help with the “pain without stain” corneal nerve pain – so a possible adjunct to the Lacripep treatments mentioned earlier.
Dr. Vidya Sankar referenced the possibility of gene therapy, as this has been increasing used for other diseases and the ability of targeting the diseases salivary glands (and perhaps the tear glands) seems within reach. Regenerative therapies are mostly available only in the form of Autologous Serum Tears for affected eyes currently, but this area appears likely to bear more fruit for our Sjogren’s patients sooner than later. Oxervate is a form of Neurotrophic Growth Factor that is already available to treat damaged corneal nerves and is in studies alongside Lacripep, to see if they can be used in this regenerative way. Neurostimulation with the nasal spray in Tyrvaya, is also under study as it may work in a similar way – but without having to add more drops directly to the surface of the eye.
In my earlier posts, I covered much of what is already available for advanced dry eye treatments common to the care of Sjogren’s patients:
https://www.eyethera.com/blog/segment-10-aampb-what-we-know-about-inflammation
https://www.eyethera.com/blog/segment-10-b-when-we-are-at-war-with-ourselves
https://www.eyethera.com/blog/not-so-secret-weapon-of-dry-eye-treatment-intense-pulsed-light-or-ipl
https://www.eyethera.com/blog/ive-tried-everything-now-what
Sjogren’s Disease: Autoimmune dry eye Part 4
When we consider the regulation of tearing and salivation (mouth moisture, AKA spit production), these functions are under the direction of the so-called autonomic nervous system. This is the collection of nerves connecting our brain with the visceral organs (basic breathing, heart beating, digestion, etc.) as opposed to the nerves connecting the brain with our skin and muscles (the somatic nervous system). Autonomic is equivalent to “automatic” and allows our body to function without conscious thought.
Sjogren’s disease can damage and “reprogram” this autonomic nerve control and according to a neurologist, Dr. Goodman, specializing in this branch of the nervous system, it can account for or cause nearly any neurological syndrome. He postulated an interesting concept – wondering if the autonomic nervous system might be able to “prime” the immune system (where conventional thought would be the reverse (that the immune system might damage or reprogram the nervous system). This would allow for what he terms “maladaptive remodeling,” where the nervous system “learns” to behave badly.
Additional thought from the GI doctors, is that the gut “microbiome” (the germs that populate our intestines and are important to our digestion, nutrition, and general well-being) may contribute to the autoimmune response. This makes sense, as the body’s reaction to germs is an innate immune response and will begin interacting at the first contact with germs – including – and perhaps especially – to those in our gut. The defenses we mount include small chemicals (cytokines) that can be released into the circulation and find their way throughout the body – including the eyes, mouth and nervous system. At the level of the gut, we find Sjogren’s causing a dry mouth, GERD – an improper movement along the GI tract resulting in reflux from the stomach and up the esophagus. The stomach can become inflamed (gastritis), and often gets “run over” by a common germ, H. Pylori, which has been associated with stomach inflammation as well as Rosacea and a variety of other ailments. Further inflammation can target the gallbladder, pancreas, liver, small and large intestines – causing havoc along the entire digestive system.
Dr. Robert Fox, a rheumatologist specializing in Sjogren’s, points out that headache is a common manifestation of this disease. Interestingly, the Trigeminal nerve – the main sensory nerve of the face, which also supplies pain feelings from the eyes – under stress from Sjogren’s, releases small protein complexes called Calcitonin Related Group Peptides (or CGRPs) that enter the brain (at the thalamus) and can dilate blood vessels which can trigger migraines and can start a cascade of pain signals including pain in the eyes and photophobia (eye pain from light). At the same time as these amplified pain signals come along, there is a second small protein (Pituitary Adenylate Cyclase-Associated Peptides, or PACAPs) that lowers the threshold to feel pain related to light, sound and muscle activity. It can also be associated with so-called “brain fog” common to those suffering from Post-Traumatic Brain Syndrome, or Post-Traumatic Stress Disorder (PTSD). This compound is also found in the tear and saliva gland regions of the Trigeminal Nerve and may release into the same (thalamus) portion of the brain responsible for sensing pain – and decrease pain thresholds (so a little pain can go a long way towards hurting).
Unfortunately, there appear to be many routes to fatigue and brain fog – including autoantibodies and depression – so there does not appear to be a “silver bullet” for fixing these problems. Dr. Kate Hackett is a PhD Occupational Therapist involved in dealing with Pain, Fatigue and Sleep. She points out that sleep apnea is more common in the Sjogren’s group – which is of interest to eye doctors, as you recall my post about the “Floppy Lids” that are commonly also related to sleep apnea – so we are more apt to refer patients for sleep studies from a common eye exam. Interestingly, the common recommendation eye doctors make to dry eye patients – about using a humidifier – appears to help patients with Sjogren’s get better sleep. She points out how important it is for patients dealing with chronic pain to get adequate rest and adequate sleep – so finding helpful tools like a humidifier can really help. Also helpful is gentle exercise and taking frequent breaks (what she calls “activity management”). Others also point to the benefits of meditation, yoga, and exercise as possible means to help “reprogram” the runaway autonomic nervous system. There is a subset of Long Haul Covid that can result in an unusual and unwanted sudden increase in heart beating (so called tachycardia) when transitioning between lying down to sitting up (called POTS – a good link here: https://www.hopkinsmedicine.org/health/conditions-and-diseases/postural-orthostatic-tachycardia-syndrome-pots ). This has also been found in some Sjogren’s patients and fortunately the same reprograming from meditation, yoga, and exercise appears beneficial for this syndrome – so all these interventions appear likely to be a mainstay of therapy for so called “autonomic dysregulation,” whether from Sjogren’s (or other diseases like long haul Covid).
______________________________________________________________________________
______________________________________________________________________________
Next week, we will explore: “what does the future look like for Sjogren’s patients?” Fortunately there are new consortiums of research activities that appear to bode well for a good answer.
Sjogren’s Disease: Autoimmune dry eye Part 3
Part 3
Sjogren’s Disease is associated with other autoimmune diseases in 52% of cases – so once I identify a patient with Sjogren’s, I always refer to a rheumatologist to assist with further diagnosis and treatments. A group of these “concurrent” diseases include:
- Rheumatoid Arthritis (attacks joints and can cause eye problems like “iritis”)
- Scleroderma (a skin disease resulting in thickened, inflamed skin)
- Celiac disease (true gluten allergy, where G.I. diseases including cancer can be triggered)
- Autoimmune Hepatitis (liver disease)
- Neuromyelitis Optica (mimics Multiple Sclerosis, but treatment is different)
- Autoimmune Thyroid diseases
- Primary Biliary Cirrhosis (another liver/GI disease)
- Systemic Lupus Erythematosus (SLE) – a complicated autoimmune disorder that can cause many diseases involving every major body system.
Some of the manifestations directly related to Sjogren’s include:
- Renal Tubular Acidosis (a kidney disease)
- Interstitial Nephritis (another kidney disease)
- Cystic Lung disease
- Cryoglobulinemic Vasculitis (where inflammation in the blood vessels can cause a gamut of body-wide illnesses).
A bit more scary, is the increased risk of Non-Hodgkin’s Lymphoma, a rare cancer of the body’s lymphocytes (part of our natural defense system). The Arthritis Foundation has a good page on this here: https://www.arthritis.org/health-wellness/about-arthritis/related-conditions/other-diseases/non-hodgkins-lymphoma-with-sjogrens-syndrome
From that source comes this:
“Not everyone with Sjögren’s has the same risk. Symptoms and factors that raise the likelihood of developing NHL include:
Enlarged salivary glands, especially if they stay swollen for months or years
Persistently swollen lymph nodes (glands) in the neck, armpit or groin
Pinpoint or button-sized areas of bleeding in the skin (usually on the lower legs) called petechiae or purpura
Nerve damage known as peripheral neuropathy
Poor blood flow to the fingers, toes, ears or knees, called Raynaud’s phenomenon
Abnormal proteins called cryoglobulins and/or gamma globulins in the blood
The number of factors you have is key in determining your risk. In people with fewer than two of these factors, the risk for NHL is less than 4%. In those with three to six of these factors, it’s nearly 40%.”
This is another reason I like to refer to a rheumatologist, as they are keyed into these (potentially many,) Sjogren’s-related issues and are in a better position to diagnose and properly refer or treat them, if they are found present.
A clip from an American College of Rheumatology meeting abstract has a good description of how rheumatologists (and other medical professionals dealing with Sjogren’s Disease) will look at quantifying signs and symptoms of the disease. The abstract I’m referring to can be found here:
When investigating how much a disease is affecting an individual, it is helpful to have a systematic way of quantifying disease activity – in part to know if that patient is progressing in a way that is better or worse, but also to help validate studies to know if a particular treatment is truly helping populations of patient with the disease. One of the greatest challenges of such studies about Sjogren’s patients, is that they are a diverse group – some of whom have multiple (other) autoimmune diseases, that there are many ways the “same disease” can affect people - and all of whom can have variable degrees of the disease (from a little to a lot) that can vary over time.
We can stratify Sjogren’s to help determine who is best eligible for disease-modifying therapies – as most therapies will target specific portions of Sjogren’s signs and symptoms – and any of them can also have significant side-effects, so patients with less illness will usually want less potentially toxic treatments. The primary disease symptoms are classified as:
- Dryness
- Fatigue
- Pain
And by a Low vs High Symptom “burden” – i.e.:
- Dry with low pain
- Dry with high pain
Disease activity can be categorized:
- Dryness (sicca) alone – without body-wide disease activity or enlargement of the saliva or tearing glands (18%)
- Predominantly dry, but with mild to moderate general body-wide disease activity (especially joint pain, blood disorders and/or gland enlargement = 74%)
- High body-wide disease activity with or without dryness (8%)
On top of this, can be multiple forms of disease affecting peripheral nerves. This is because Sjogren’s can also primarily attack these smaller nerves and affect our sense of balance, our ability to sense or feel things – or can result in a normal ability to “sense” even while depleting the tiny nerve fibers in skin and in the surface of the eye (leading to surface problems and can wreak havoc on those already suffering with dry eyes).
Next week, I’ll focus on more specific issues associated commonly with Sjogren’s and some of the advances in treatments that are underway…
Sjogren’s Disease: Autoimmune dry eye Part 2
Sjogren’s Disease: Part 2 – how it can affect us… Let me count the ways!
In a 2021 United States of America survey by the Sjogren’s Foundation, where they got 3,622 Sjogren’s afflicted patients from this country responding, the age groups who reported varied from 18-94 years of age. Over half believed they had symptoms of their Sjogren’s disease before the age of 35 years, with 16% having symptoms before the age of 18 – so this disease can start early in life! Over 60% had a family history of autoimmune diseases, so there appears to be a genetic predisposition (though clearly there are many cases where there doesn’t appear to be that obvious of a genetic link).
Importantly, while eye dryness was the number one issue for most, over 80% had at least one diagnosed nervous system-related health condition, which could include:
Anxiety or depression (50%)
Brain Fog (47%)
Neuropathy (45%)
Migraine (32%)
Fatigue (25%)
The Sjogren’s Foundation reported 20 clinical treatment trials underway, with 3 of them already in phase 3 testing (so looking near to being approved by the FDA for broader treatment of Sjogren’s Disease). As more treatment protocols become available, it will become increasingly important to accurately diagnose the disease, so it can be staged and properly treated. Treatment will commonly require a competent team approach, usually involving the dry eye specialist for detection and eye treatment, an oral surgeon coupled with a good oral pathologist to help with detection and treatments that may involve a diagnostic biopsy of the mouth’s saliva glands and perhaps opening the saliva ducts inside the mouth, dentists to take care of the frequent cavities and dental decay acquired from a dry mouth, and rheumatologists to aid in diagnosis, staging, and treatment plans related to Sjogren’s and to the many, often associated autoimmune diseases that can run in concert with it. Gastroenterologists, neurologists, pulmonologists (lung), nephrologists (kidney) and sometimes, endocrinologists (especially thyroid) and oncologists can also be needed - depending on the range and severity of the disease.
Diagnosis can be difficult, as blood tests are not always reliable and may miss it (though a positive major antibody test – the so called “Ro” - is considered diagnostic, it is sometimes not found in patients with active disease). Ultrasound of the saliva (the “spit” or “salivary”) glands, including the large parotid glands, may help point to the diagnosis as there are many classical findings (as can also be true for MRI, CT scans, and in the case of lymphoma – a relatively rare cancer that can be more common in some patients with Sjogren’s, then PET scans can be helpful) – but a biopsy of affected saliva glands is still considered the most definite way to diagnose if the blood tests are negative (and requires a good pathologist to “read” the results, as it is easy to over or under diagnose).
So far, unless a patient of mine has very poor “sprinkler system” output (as measured by a very low Schirmer’s test) as well as a history of a very dry mouth (like not being able to swallow a dry saltine-type cracker without water to wash it down), I generally don’t go looking for Sjogren’s with the blood tests - unless there is a poor response to standard initial treatments for their dry eyes. This is because so far, there has not been an acceptable protocol for treatment beyond the eyes – leading me to not go looking for a disease we don’t have a good “fix” for. Adding a lip biopsy to a negative blood test didn’t make sense for the same reason. That may soon be changing as the newer treatments become available, though any patient with severe disease will usually be detected early and referred to the appropriate specialists – as even the imperfect treatments available now are still better than allowing Sjogren’s to “run rampant” in a severely afflicted individual.
Future posts will elaborate on some of the ways Sjogren’s Disease can attack specific body parts apart from the eyes, and I think you’ll soon realize why a team approach is required – since Sjogren’s is so much more than a “Syndrome!” If you or someone you know has Sjogren’s Disease (often referred to as Sjogren’s Syndrome”), then please make sure they check the Sjogren’s Foundation website, since they offer invaluable information and they help keep us all updated on breaking news about this challenging disease.
https://sjogrens.org/living-with-sjogrens?gclid=CjwKCAiAxP2eBhBiEiwA5puhNcqJeHtH9tfIpr769Pb7jjS2_qGTgvtSpk0Q25Fv9dFHjMssbzuykBoC5REQAvD_BwE
Sjogren’s Disease: Autoimmune dry eye Part 1
Sjogren’s Disease - or; When our immune system starts throwing “smart bombs” at our water-producing glands and what that can mean to our eyes (& to our life!).
Until relatively recently, Dry Eye Disease was called Dry Eye Syndrome – probably for several reasons. First, is that we didn’t understand it very well (not to imply we now understand it particularly well – just “better”). Second, saying “disease” sounds more “harsh” or “serious” – while “syndrome” somehow seems less severe or serious - and since we didn’t have a lot of understanding – or ways to treat it - it seemed better to “downplay” it.
This terminology also applies to Sjogren’s Disease, as it was also referred to as “Sjogren’s Syndrome” until relatively recently, perhaps for many of the same reasons. While we now understand it better, we still have a long way to go – and since it can have a huge impact on our being, it is good to know that there are many studies underway to help improve our understanding and give us more tools to treat it.
Early in my posts, I covered the “accidental” damage to our tear glands that commonly occurs when our eyes become dry and irritated, as irritation begets inflammation and inflammation leads to damage to our tear glands. As the glands become damaged, we get more dry and more irritated, which leads to more inflammation and more dryness – the so called “vicious cycle” of dry eye disease. As our immune system spools up, it can act like “gas on the fire” of this vicious cycle.
Sadly in the case of Sjogren’s Disease, our immune system becomes more confused and starts making antibodies that attack the water-producing glands throughout our bodies “on purpose” (versus the more typical “accidental” damage from dry irritation) and can become a hydrant of gas on that fire. This affects our eyes by drying up the water in our tears and since water makes up most of a healthy tear, the tear volume drops and eyes suffer.
But Sjogren’s frequently goes far beyond affecting our eyes, as the white cells (Lymphocytes) from our immune system can also attack our nerves, our organs and especially, our gut. This post serves as a basic introduction - and for future posts, I’ll cover more details about how broadly this can affect us, current aspects of diagnosis and some of the commonly accepted current treatments – but will attempt to touch on some of the newer approaches and possible treatments being investigated.
As these immune cells (Lymphocytes) go after nerves, they will cause an “autoimmune neuropathy” – where nerves can become weaker and lead to numbness or pain (and sometimes, degrees of both). In an earlier post, I noted how corneal nerves are the “maestro” that conducts the “orchestra” of tear production and of the delicate dance of cells that constantly turn over and renew the surface of our eyes. Poor tears can weaken that surface, but when the cells lose their “marching orders” the surface can get very rough and damaged. These eyes may need every trick in our book to survive. Commonly, this includes some degree of anti-inflammatory drops like Cyclosporine, Lifitigrast and topical steroids, biologic support from Autologous Serum Tears and Amnion products and higher levels of attention to ancillary dry eye issues like Meibomian Gland obstruction, Rosacea-related inflammation, blepharitis, allergies and surface issues pertaining to the conjunctiva and eyelids.
I harp on use of preservative free artificial tears (so we don’t punish the tear glands and eye surface with harsh chemicals designed to kill germs that may gain access to the bottles through air or contact of the tip with our eyelids or fingers) – but as a final portion of this post, I will also mention that this opens the door to bad germs gaining access through contamination at the factory level – as appears may be the case from this CDC notice: CDC Urges Discontinued Use of EzriCare Artificial Tears (as they may be the source of some terrible eye infections and possibly one death)! Stay tuned for more…
52.1429 weeks in a year - and this is #52 of my Dry Eye Posts!
Another Happy New Year to you. In reviewing my posts since my start 12/29/21, I noticed this is officially #52 and since Google says there are 52.1429 weeks in an average year, I guess this closes out a full year of my posts. I took the opportunity over the weekend, to read each and every one of these posts and I noticed the common theme - Tears are important as they serve as the “clear blood” serving to support the living surface of our eyes. Blinking is the “heartbeat” that constantly renews and re-distributes that “clear blood” so the surface can stay healthy with those fresh tears.
I also noticed that while I repeat certain information in many of my posts, it comes down to the mainstay of how to help keep tears healthy - so they can support that living surface through the thick and thin of modern life. Such life now lasts longer than prior generations - yet we use our eyes more than any generation before us, thanks to the “digital world” we live in. That kind of stress is bound to show up in a diverse array of ways and can account for the many signs and symptoms relating to unhealthy tears. We dry eye specialists refer to unhealthy tears as “Dysfunctional Tear Syndrome” but call it “Dry Eye DIsease” to our patients, friends and non-dry-eye-specialist colleagues. We refer the outcome of those dysfunctional tears, as “Ocular Surface Disease,” and many of us have devoted much of our careers to better diagnosing and treating it.
Once we accept that tears equal “clear blood,” then it is easier to accept that when tears go bad, the surface of our eyes will “go bad.” Just as “bad blood” can’t support our bodies to stay healthy and will lead to “disease,” this means bad tears will lead to “Dry Eye DIsease” (or whatever we chose to call it).
For any of you in doubt about whether you may have dry eye disease, I refer you back to my first posting, December 29, 2021, https://www.eyethera.com/blog/rn9p8ouyjzjhyfpkvrysxjx28no0q8 where I posted my introduction to dry eye disease and a simple 20 second “test” you can do at home to help you. If any of you find the test pointing in the direction of Dry Eye (or Ocular Surface) DIsease, then if you haven’t done this in a while (as I had not), I will suggest you read through my posts from the start, to present day. I think (and hope you’ll agree) I’ve done a reasonable job at putting it all into some perspective - at what I aim to be the “average patient level.”
Launching my postings into 2023, I will do my best to continue this tradition and help bring newer thoughts, technologies, treatments and perspectives to what I can share. I realize that many of my readers are already my patients, friends, colleagues and family - and I hope to “spread the word” through each of you, to your patients, friends, family and colleagues. Let’s help “stamp out” dry eye and ocular surface disease together!
Do blue blocking glasses help with dry eyes?
As a dry eye specialist, I’m often asked if wearing blue blocking glasses (or adding blue blocking filters to computer screens) can help or prevent dry eye disease. The short answer is possibly, but the better answer follows.
Scientists point to the regulation of our sleep schedule being dependent on a schedule that evolved over eons and was regulated by the sun. Long before we had homes with electricity, we commonly lived in caves or other primitive structures and the day began around the time the sun came up and ended around the time the sun set (or our campfires went out).
The “blue sky” we see in daylight is a strong “wakeup” signal that would prepare us for a day of hunting and gathering that could sustain us and allow our species to survive and thus evolve. At night, a small gland in our brain, called the pineal gland, would begin making melatonin around the time the world went dark and prepared our bodies (and brains) for sleep. As the melatonin seeped into our brain, it functioned as a type of sedative that allowed us to have the sleep-related rest that prepared us for the following day.
Today, our day often begins with an alarm (perhaps set on our smartphones) and with the electric lights coming on – often hours before a full sunrise. Conversely, our day often ends many hours after the sun sets – and during this “artificial daylight” our brains are denied the gradual buildup of that natural sedative (melatonin) that the bright blue sky would stave off so we can hunt and gather. Unless we use programs and filters to block the blue light we see while staring at all the screens that seem to rule our lives, this is a strong source of that “wakeup signal” that makes sleeping difficult.
Sleep is incredibly important to our health in general and to our eye-health in particular. Resting with closed eyelids can help restore the living surface of our eyes, as they are no longer exposed to the drying atmosphere - and the delayed blinking - caused by staring and visually concentrating while awake. Video screens (phones, computers, tablets, and laptops as well as TVs) are a great incentive to staring – and as I pointed out in earlier posts – staring is like giving your eye’s surface a “heart attack” as blinking is the “heartbeat” that churns the “clear-blood-like product we call a tear” over on the surface of your eye to sustain and support it.
The principal benefit of blue-blocking-glasses (or screen covers/filters) appears to be the return of the melatonin-related regulation of our sleep cycle – and the return to better sleep and better health. This is especially useful once the sun sets, so some computers have settings where you can reduce the blue in the screen automatically. Lighting can be dimmed around the house after sunset and aiming for the number of hours of sleep you need can be an easier task.
The limiting of screen time, the 20/20/20 “rule” of taking 20 seconds every 20 minutes to look 20 feet or further away (and doing some strong blinking to promote the function of the lid’s oil glands) is also helpful to maintaining healthy tears and therefore healthy eyes.
So do blue blocking glasses help dry eyes? If you, like most of us, spend “too much time” after dark, staring at screens that have the full spectrum of natural colors (including that bright blue-sky blue), then definitely consider blue blocking strategies and get some sleep!
More on MGs (the tear oil glands)
In dry eye patient chats, I commonly come upon questions like - “My doctor says I’ve lost a lot of my Meibomian Glands. How many MGs do I need to have a good tear?” And: How fast can they disappear?” “How do I get them back?”
Dr. Donald Korb is the Optometrist who invented Lipiflow (the first well-sorted tool to provide a good heated expression for obstructive MGD). He is a great observer and excellent researcher. He is also the one that told me 6 good MGs/lid is sufficient to support an adequate tear (usually measured by the tear break up time and lack of dry spots on the cornea). I don’t believe this has been supported in peer reviewed studies but based on his expertise and my clinical observations, I can say that I believe this to be true. That’s good news for those struggling to keep 6 or more well functioning glands. This doesn’t necessarily speak to the quality of the oil, the constitution of salts and proteins nor the volume of water that is the bulk of a tear. It also is bad news for patients who don’t yet have a handle on the number of glands they still have, as most people have 25-30 glands per lid at birth. If you’re down to your last 6 good glands, life is good until you lose one more gland. So the short answer is that it is best if you can hang onto more than 6 and keep them in good shape.
It would be unusual to lose 50% of the MGs in 6 months (or even a year, since it appears to take years-to-decades for the average dry eye sufferer to see major losses) - but in cases where blinking is severely impaired - like a Bell’s Palsy - or in cases where medications like Accutane have been used, I believe it may be possible to lose as much as 50% in less than a. year. Sadly, the imaging used to detect the glands is far from perfect and the state of MG activity appears to greatly influence how "white" (and therefore detectable) they appear on InfraRed photography (the standard way of imaging them). If you can support them with adequate Omega Oil supplements, warm moist compresses with "lid crunches," blink exercises and good lid hygiene after ensuring adequate purging of obstructions, then I have found it is possible to see many of these ghostly MGs "bounce back."
Regeneration of the glands remains controversial, but it does appear that glands that are not “too far gone” can bounce back if given the chance. In general this means adequate unclogging and then adequate “homework” as I outlined in earlier postings. IPL appears uniquely suited to stimulate them, and Maskin Probing is sometimes required to sufficiently unclog them, but a good heated expression is often needed with or without the probing and IPL treatments. Best to work with a good dry eye specialist and do the homework.
How Safe and Effective are Home-Based Radiofrequency and Light Treatments for Dry Eye Care?
Happy New Year! I thought it would be appropriate to start the new year with a common thread among some dry eye sufferers I’ve advised over the past year. The common question is – since office-based treatments are so expensive and because some similar technologies are now being offered for self-treatment home care – why can’t I just buy a radiofrequency unit and a light-based unit, and do my own treatments? These treatments could perhaps replace some office treatments, or be used as an office treatment “extender,” or optimizer?
When a particular RF unit was singled out, I found an Amazon link to an eerily similar device for $99. There was very poor grammar in their marketing brochure, suggesting a poor understanding of English language. Some foreign countries have substantial road blocks to product liability and if they fry some eyeballs, there isn’t much recourse. A FB post I did to address a question from a dry eye sufferer helped explain my take on these cheap, “fix it at home” technologies:
I can’t speak to specific “Over The Counter” (OTC) products like this one, but generally speaking, the aim of RF (off label, as it has yet to be studied and approved for this use by the FDA), is to heat directly over the eyelid area, to melt and allow adequate expression of the waxy obstructions in the oil glands of the tear system. Because RF can penetrate deeply through the skin and eyelid tissues, I’ve found it extremely useful for this purpose. I also used special thermal imaging cameras to track this temperature and found if you don’t get to the common “melting point” of the waxy plugs obstructing these glands (around 42-43C) then you never really get that adequate expression. That same temperature can also affect the cornea or clear “window” of the eye, as it resides directly under the lids. Doctors using this technique will use special eye shields to protect the cornea and to assist in the expression of the waxy obstructions. The OTC tools I’ve seen do not appear to have a temperature monitoring system (it goes off by time and not the temperature) so it is hard to know if they can unclog the glands. They also doesn’t have anything to protect the cornea if you do get it that hot, so I personally cannot endorse them. As far as getting the aesthetic benefits, the prescription strength RF devices have good scientific studies to back up true clinical results we see but I didn’t see any such studies for the OTC units. Any form of deep heat can temporarily improve the appearance of fine lines and wrinkles by swelling the skin, but the long-term improvement comes from the specific stimulation of the cells that make and repair collagen and elastin. I’d be interested to see peer reviewed, dry eye studies using these home-based, OTC units. I’m working with some RF companies (as are other doctors) to increase acceptance of RF worldwide for dry eye treatments, which requires ongoing studies and training specific for dry eye diseases.
Low Level Light Therapy (LLLT) is a world-wide growing trend, using relatively low levels of light in certain spectrums found to benefit a variety of medical ailments. LLLT encompasses a wide range of light energies and spectra and has many scientific studies to support biological influences that may be beneficial for a wide range of problems (& some units may have been FDA approved for the treatment of those problems - so the manufacturer can claim it is FDA-certified) – but as far as dry eye disease goes, it has no where near the level of study (nor specific FDA approval for that specific indication) as many other treatments, including IPL, which was approved over a year ago, specifically for the treatment of dry eye disease.
There are numerous anecdotal reports and some limited published reports of dry eye benefits, so some companies are selling these units to eye doctors – and while there are an increasing number of those doctors using this technology for the purpose of treating dry eye, I have not been able to find enough peer reviewed, scientific data to support the safety and efficacy of LLT for dry eye-related disease. At least the majority of these office-based “eye” units have been specifically tested for eye safety and have USA-based companies representing them, – so product liability is likely to be well regulated. Units you can buy and use at home can provide over 10,000 lux of light energy – and that amount of light energy is certainly sufficient to cause harm to an eye if not appropriately shielded. Filters can bring that light into a spectrum like an IPL’s when treating dry eye – so while there may be efficacy for some units – the proof of safety and how well they work remains to be sufficiently validated before many of us would recommend it for our patients using office-based care – and even more so for home-based treatments.
As usual, I recommend working with a dry eye specialist who can offer a range of proven dry eye care treatments, who can take some time to answer your questions and provide a well explained treatment plan specific to your dry eye needs.
Here’s to a healthier, happier 2023!
Why do some people produce “pasty meibum?” PART 4
Part 4:
This brings us to the issue of lid hygiene. Germs feast on our oils and Demodex likes to feast on the germs fat on our oils, as well as feasting on those oils, themselves. Rosacea-related - and many other cases of dry eye disease-related - inflammation is commonly stirred up by those germs and particularly by the Demodex mites involved with those germs. Based on what I've read about Demodex and rosacea - and given the near pandemic of rosacea I find in the northeast, I think there is good reason to prescribe anti-Demodex therapy for those who have rosacea and/or MGD. (I've heard statistics that suggest that we may all get infested with Demodex if we live long enough – approximately 30% have it by age 30, 50% by age 50 and 90% by age 90.)
I also find it rare to see rosacea patients who don't have some degree of evaporative dry eye disease. (the form of dry eye that comes from too little, or the wrong kind of oils in our tears). Though many have thin, clear oil (if scant), I find frequent soap-suds-like bubbles in their tear film - presumably from bacteria. Demodex can add inflammatory elements to those “clear oils” - making the oil more like “kerosene,” than like the “extra virgin olive oil” you’d prefer in your “salad dressing.” Because of the good luck I've had with Cliradex, I have been reluctant to abandon its use in select cases - but I also find that the Avenova iLid cleanser can work well, coupled with ZocuWipes – and is less irritating to the sensitive skin of most of these rosacea patients. I routinely package these in my dry eye “kits” that can be additionally custom tailored to meet the needs of each patient I see. Topical Ivermectin has shown good activity against Demodex and there is a pipeline drug, likely coming to market within the year. IPL, along with improving the flow of oils (with the many tools available for this) both help control Demodex, along with lid hygiene. Combined with pure Hypochlorous Acid sprays, this is for most) an effective way to control bacteria and mites from adding to dry eye (and eyelid) misery.
To combat this problem, I think we need to better educate patients. Just as we teach kids to eat a less sugary diet, brush and floss their teeth and go to the dentist regularly to save their teeth, we need to do something similar for encouraging better blinks, diets rich in the essential Omegas, physical activity/exercise and lid hygiene to save their eyes. Procedures that melt and express these waxy oils are necessary in the more advanced stages, but if caught early, I believe we can largely prevent MGD - or at least better control it. I’ve used Dr. Korb's technique of debridement of the lid margin as an adjunctive tool to his Lipiflow technology, though as I’ve noted, I’ve published on modifications of this with some off-label use of radiofrequency for a more customizable expression and often combine it with a BlephEx lid hygiene treatment and Intense Pulsed Light Therapy (see my earlier posts on this). It is ironic that the nation leading in health and technology is poised (in some part due to our computer-dependent workforce and lifestyles) to be a nation of irritated, dry eyes - as we fail to properly care for our eyes even as we over-use them and - thanks to every other aspect of modern medicine - begin to outlive our MGs and their basic but critical tear functions. The “homework” I prescribe (and have endlessly posted on) remains the mainstay of what has - for the majority of my patients - been an effective way to support and promote the Meibomian glands and to prevent the “pasty Meibum” that is so common a cause of obstructive MGD and resulting evaporative dry eye disease.
Why do some people produce “pasty meibum?” PART 3
Part 3:
It is clear that there is a significant difference in the composition of oils from those with MGD and those without - and it appears that bacteria may play a major role in some of these differences: I quote from a scientific paper (and add interpretations) below:
"Using the compiled data, the team semi-quantitatively revealed the variety of FAs and OAHFAs (Fatty Acids or FAs and (O-acyl)-omega-hydroxy fatty acids or OAHFAs = building blocks of tear oils) present in MGD-affected human meibum. Overall, they identified 161 molecular species. Of these, 100 were long-chain FAs containing 12 to 37 carbons, which is a marked increase in comparison with other detection methods. The remaining 61 species were long-chain OAHFAs 34 to 56 carbons. The researchers note that a wider mass range could result in identifications beyond the 37-carbon threshold for FAs but indicate that this study is the first report of large numbers of very-long-chain species in human meibum (tear oil). Given the rare nature of species longer than 35 carbons in blood, skin or cell samples, this finding confirms the unusual lipid composition of meibum (tear oil). Interestingly, the team also detected odd-numbered carbon-chain FAs, which previously have been linked to bacteria. Mori et al. recommend further investigation into a potential link between this finding and possible bacterial infection in the eyelids of MGD patients."
(This is one of the reasons I stress good, regular lid hygiene to my dry eye patients.) From: http://acceleratingscience.com/proteomics/meibum-lipid-composition-in-dry-eye-disease/
Once one thinks about the normal, wide range of complex oils in the healthy, human tear, it is easy to understand how difficult it will be to create a sufficient “tear substitute!”
Now that I look harder at my routine patients, I find MGD to be nearly ubiquitous - and prevalent even in those as young as early teens (& probably earlier - I just no longer see young kids in my practice). I think this begins with poor blinking (a subconsciously "learned" response that is encouraged by use of computer-related activities like smart-phones, tablets, video games, computers and the like - and discouraged by outdoor play, where bright lights, wind and vigorous activities encourage better blinking). Inactivity may also lead to reduced blood flow in the lids that may reduce eyelid temperature. Poor diet (the high levels of processed foods in the America diet are said to have reduced healthy Omega oil intake by over 95% compared to 100 years ago, when such processed foods hardly existed) needs to be reversed - with a better focus on good eating habits and proper supplements (I like the MaxiTear Dry Eye Formula, which comes closest to Hydroeye as an all-in-one, based on the work of Drs. John Sheppard and Stephen Pflugfelter, but includes a bit more fish oil, some Curcumin to help fight inflammation and an enteric coating to prevent fishy, after-taste burps). Once oils become stagnant, they become the “buffet table” for common skin germs, who feast on the oils, create inflammatory byproducts and lead to the vicious cycle of dry eye disease.
Part 4 focuses more on how to correct this…
Why do some people produce “pasty meibum?” PART 2
Part 2:
Fortunately, not all the tear oils come from the MGs – I quote from (and partially interpret) a scientific publication (below) regarding the composition (and sources) of tear oils.. For those not interested in all of the science, the take home is that much as we regard the Meibomian Glands as the sole provider of tear oil, the reality is that there are other likely sources that make significant contributions. The hopeful news (from my perspective) is that some of these alternative oil sources may be able to be amplified in some cases of reduced (or absent) MG function – to offset the deficiency of the MG dysfunction. I believe I’ve witnessed this in some cases where there do not appear to be any residual MGs left in any of the lids – yet the function of the tears, and general health of the corneas, appear clinically adequate (and may have little-to-no dry eye symptoms) …
"There is no doubt that the meibomian glands are a prominent source of lipids for the TF (Tear Film). However, it would have been a mistake to exclude from consideration other likely sources of lipids (oils), such as conjunctiva, cornea, and AT (Aqueous/watery Tear) produced by lacrimal glands. Earlier publications provided some clues about possible differences in lipid (oil) compositions of MGs and AT and similarities in the AT samples collected using the microcapillaries and Schirmer test strips.27 34 35 Our current HPLC-MS (fancy scientific analyzer) data showed that lipids of aqueous tears are more complex than meibomian gland secretions, necessitating a more cautious interpretation of the roles of the latter in tear film physiology. The observed presence of lower molecular weight compounds with m/zvalues between 500 and 600 and the detection of the large quantities of the compounds with higher polarities than typical meibum components suggest a more complex TFLL (Tear Film Lipid Layer) composition than the one based only on MGs. Therefore, a detailed comparative lipidomic analysis of specimens obtained from different sources, determination of the structures of the newly detected lipid species, and evaluation of their possible physiological roles are in order." (http://www.iovs.org/content/49/9/3779.full) I remain surprised that there has not been further significant research and advancement of knowledge regarding these “alternative producers” of tear oils and look forward to results of such research.
Why do some people produce “pasty meibum?”
Why do some people produce “pasty meibum?” (A Root Cause of MGD that looks like strings of toothpaste or spaghetti - rather than thin, clear oil when expressed from these oil glands. This “clogs” the glands and creates obstruction.)
Some years ago, I was asked by a colleague about why some people produce “pasty meibum.” I wrote a long diatribe and when I saw a related question recently, I dug this answer up and thought I’d share.
Part 1:
Some of my answers would be somewhat modified today. (As most of you know, I’ve published on off label use of RF (radiofrequency) over Lipiflow and for addressing conjunctivochalasis, Zocuwipes over TTO related cleaning and Maxitears over other oils supplements - FD, consulting RF companies, part owner of the eyeThera company that makes the shields I use for RF expression and consultant to the Zocular company making the Zocuwipes).
My 4-part answer attempts to address that million-dollar question.
The Tear Science folks (initially headed by Drs. D. Korb, C. Blackie, et al - but now owned and operated by J&J) would include poor (partial) blinking in that answer, as that appears to be a major cause of stagnation of the oil producing eyelid glands (MGs). When stagnant oil becomes exposed to air, salts and the acidic breakdown products of bacteria and their oil-digesting lipases - it turns to soap and solidifies. Where normal MG (Meibomian Gland) oils are liquid at body temperatures, these harder oily complexes become wax-like and block the glands. The back-pressure appears to induce withering (or else they go on to produce styes). Of some interest is Dr. Korb’s finding that the temperature of the eyelids in patients with Meibomian (oil) Gland Dysfunction (MGD) is "colder" than those who don't have MGD. As far as I know, no one has been able to explain this phenomenon (though Dr. Korb points out that athletes have higher lid temperatures and appear less prone to this disease), but lower temperatures would also lead to solidification and blockage. Dr. Korb demonstrated to me the capillary attraction produced by the lids as they separate after a full blink. This engages the oil squeezed out by the action of the lids coming together with enough pressure to dispense micro-droplets onto the lid margin. Tiny vertical indentations in the lid margin assist in this backward and upward movement of oil - unless a waxy varnish obliterates these little "riverbeds" and occludes the openings. This is one reason I like to “debride” (scrape off) this waxy varnish as a part of my dry eye exam as it aids my diagnosis and may help in treatment of some with serviceable glands that are otherwise “dysfunctioning.”
Part 2 addresses other sources for tear oils and digs into what these oils are.