Blog
Rosacea and Dry Eyes Part 7 - the mental aspects of rosacea.
Updates on the Risk of Neuropsychiatric and Gastrointestinal Comorbidities in Rosacea and Its Possible Relationship with the Gut-Brain-Skin Axis.
Rosacea and related dry eye can have a host of impacts on a patient’s mental status (which also needs to be addressed and in many cases, also treated):
(adapted and annotated from: Woo YR, Han YJ, Kim HS, Cho SH, Lee JD. Updates on the Risk of Neuropsychiatric and Gastrointestinal Comorbidities in Rosacea and Its Possible Relationship with the Gut-Brain-Skin Axis. Int J Mol Sci. 2020 Nov 10;21(22):8427. doi: 10.3390/ijms21228427. PMID: 33182618; PMCID: PMC7696644.)
-Chronic pain syndrome (chronic erosive and corrosive impact on the surface of the eyes, with secondary irritation, inflammation) – eyes are important and help define our relationships to people, places and things. When eyes hurt, we may act out – or withdraw – with either reaction likely to affect our mental state.
-Anxiety/Body Dysmorphism (most have a degree of red eyes/lids/red face, many have frequent chalazia/styes, some have pustules (whitehead zits), papules (red bumps/zits), more rarely a phymatous (swollen) reaction. These changes can make us nervous and can negatively affect the way we see ourselves (dysmorphism).
-Depression (chronic anxiety, poor sleep, chronic, progressive nature of the disease) and slow, sometimes painful & painfully slow progress from treatments, with variable effects on vision, work performance, family life and the ability to enjoy common outdoor activities from weather impacts).
-High prevalence of GI issues associated with Rosacea. (poor absorption, increased circulating inflammatory mediators and abdominal pain with irregular bathroom habits and related social stressors).
Psychological aggravating factors such as stress, anxiety, personality issues with excessive feelings of shame and guilt, and social anxiety secondary to easy blushing could worsen the flushing in patients with rosacea and be a factor involved in the vicious cycle of rosacea.
-Known association with cardiovascular disorders (hypertension and coronary artery disease – adding additional psychic stress).
-Another chronic neurovascular disorder, migraine, shares a variety of clinical features with rosacea. Migraine and rosacea both have features of chronic, recurrent paroxysmal episodes with disabling symptoms in the trigeminal nerve (the nerve responsible for sensing pain in and around the eye as well as areas of the face). Indeed, Tan et al. first reported that 44% of the patients with rosacea had experienced migraines. Ocular rosacea appears to have a special connection to migraines, in that the more extreme “Phymatous” version of Rosacea is not commonly associated with migraine and Ocular Rosacea, is. It is also true that many of the “triggers” for rosacea are shared as equal triggers for migraines (especially the “vasoactive” foods like spices and alcohol, as well as extremes of hot and cold weather).
-Migraines independent of rosacea can be disabling with its own major effects on life-balance.
Because inflammation is central to many disease states, it should not be a stretch to understand that other neurological illnesses, such as Parkinson’s and Alzheimer’s Diseases are also more common in rosacea patients - though I should point out that there is much for medicine to learn about the intricacies of these “associations” and just because one has one disease, does not mean one is destined to acquire others.
This and future posting should help us understand why it often takes a village to best help our rosacea patients - with eye-affected ones requiring substantial assistance from eye care professionals.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Rosacea and Dry Eyes Part 6 - the Tetracyclines (including Doxycycline and Minocycline)
Fast forward 40,000 years from cave paintings (or so) and we have a better understanding of rosacea, including the biological underpinnings and stressors that drive this response today. Adapting and annotating from a Johns Hopkins Review Article: ‘stressors, including ultraviolet light from the sun, microbes (Demodex has stepped into the spotlight lately - see my post here: https://www.eyethera.com/blog/demodex-the-tiny-mite-with-a-big-effect-on-dry-eye-disease ), trauma, emotional stress, and some hormones, may stimulate the release of “neurotransmitters” and contribute to the dilating blood vessels, flushing, and increased skin sensitivity, stinging, itch, and lower pain thresholds in patients with rosacea. Interestingly, pain fibers have been found to be increased in erythematotelangiectatic rosacea. Ion channels that regulate cell functions are (over) expressed in rosacea, on nerves, corneal surface cells, mast (allergy) cells and/or immune cells, making them highly reactive to thermal, chemical and/or mechanical stimulation.’
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5821167/#cit0003
This was echoed and elaborated in a more recent review of Rosacea: “Dilation of lymphatic and blood vessels with exposure to extreme temperatures, spices, and alcohol has been observed in rosacea.” and “in addition, expression of matrix metalloproteinases (involved in inflammation) and vascular endothelial growth factor (invoved in blood vessel growth) is increased in rosacea. In rosacea, microbes may trigger activation of the immune response. This hypothesis is supported by an increased number of organisms, such as Demodex folliculorum on the skin and helicobacter pylori infection in the gut of patients with rosacea.”
https://www.ncbi.nlm.nih.gov/books/NBK557574/#article-28642.s5
The reason this is important, is that one of the more accepted treatments for rosacea is antibiotic therapy from the Tetracycline class (including Doxycycline and Minocycline). These antibiotics can interfere with the matrix metalloproteinases (reducing inflammation) and can kill helicobacter pylori (the bacteria commonly linked to stomach ulcers and thought to potentially lead to stomach cancers). These antibiotics are relatively cheap, often covered by health insurance plans and can be effective at reducing the skin and eye redness, sensitivity and irritation from rosacea. So why isn’t everyone with rosacea on these antibiotics?
Probably the number one reason is that these antibiotics don’t know the difference between “good” and “bad” germs - they simply take out any germ that is susceptible. This has the potentially adverse effect of encouraging resistant germs to “take over.” These can be yeast (not being a bacteria, they aren’t affected by these antibiotics and require specialized anti-yeast” medications to recover). Other germs with a drug-resistant profile are increasing in numbers and in their capacity for harm - but since they are resistant to most antibiotics, they pose a greater threat once they “turn bad” and cause diseases.
Fortunately, at the (low) dosages commonly recommended for treating rosacea, the effect on gut germs can be limited and this can potentially circumvent some of the harsher issues. But there are other issues that also need to be addressed. Because they are acidic in nature, they can be a little rough on a sensitive stomach - so taking them with food is often recommended. However foods containing calcium can bind to the antibiotic and make it difficult to absorb it (so it can run through the gut without getting into the bloodstream, where it would be needed to help fight facial and ocular rosacea). Probiotics like yogurt can help restore healthy germs to the gut after the antibiotic knocked them out. But yogurt is high in calcium, so while it is a good food for those taking these antibiotics, it is important to stagger the yogurt (or other calcium-rich foods) 1-2 hours before or after the antibiotic to allow optimal absorption. It is also advisable to not take the antibiotic right before bedtime, as it can get caught in the esophagus (before getting to the stomach) and cause ulcers or irritation (the stomach is naturally acidic and can usually easily handle it).
Add to that, the fact that it can negate the effects of birth control pills - but also is known to affect fetuses badly (causing birth defects) - so women of childbearing age need to be especially careful not to get pregnant while taking these antibiotics. It is also worth noting that patients who can sunburn - will be more prone to sunburning while taking these antibiotics. (It increases the damaging effects of Ultraviolet light on skin treated with the Tetracycline-type antibiotics - so it isn’t the drug that sunburns you - it is the sun that sunburns - just more easily). This means those on these antibiotics need to be extra careful when exposing themselves to the sun (covering up and wearing appropriate amounts of sun blocking lotions or creams). Taking them with a tall glass of water and a bit of bread or fruit after dinner - but at least an hour or two before bedtime can often allow them to do their best without significant stomach or lower gut side effects. Taking them at night can also limit the sunburning - (when the dose in the skin is the highest when there is no sunshine to sunburn.)
Lastly, it is possible to become allergic to the entire Tetracycline group from taking any one of these related antibiotics. This can be especially problematic for those who really need this particular antibiotic (like those with Lyme disease - where this is the preferred first line treatment against the Lyme organism). While the common allergic reaction is a rash, more severe allergies are possible - so when in doubt, best to immediately contact your doctor - or if not immediately available or in severe cases, to go immediately to the nearest Emergency Room.
Despite these potential adverse events and special considerations, Tetracyclines can be a good fit for many patients and side effects are usually easily mitigated - so I consider them on a case by case basis. There are also many treatment options apart from the Tetracyclines and it is best to work with a good dry eye specialist to determine what is best for you. We will delve further into this in future posts!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Rosacea and Dry Eyes Part 5 - how did Rosacea “happen” to me?
Representation of a wild bovid, the Banteng, made in ochre, discovered in the Lubang Jeriji Saléh cave, East Kalimantan, Borneo, Indonesia, dated to 40 ka. Discovered in 1997 by Kalimanthrope (Pindi Setiawan, Luc-Henri Fage and Jean-Michel Chazine), it was dated to -40,000 BP in 2018 by Aubert & ali. and remains one of the oldest samples of figurative rock painting. This image appeared on Wikipedia's Main Page in the Did you know? column on 17 December 2018.
I’ve mentioned in a (much) earlier post that I have Rosacea, too. In thinking about how this might have “happened,” I like to think in evolutionary terms - and since it affects me, I like to think of it as a form of “higher evolution;)”
One of my premises about how dry eye evolved, begins with the notion that our great-great-great ancestors (thinking many hundreds of thousands of years ago and beyond) were characterized as the “hunter-gatherers.” These simple folk subsisted off the fish, nuts and seeds - or animals that ate the same fish, nuts and seeds (note the above cave drawing) - because way back then, there apparently was little else to eat back then. Those same folk generally lived in caves or some form of hovel (apart from the aristocracy that undoubtedly existed even then) - and lacking modern degrees of hygiene, one can assume these places were not up to today’s standards of cleanliness.
To survive as a species, we spent a lot of time hunting, gathering and procreating - but living in what we - today - would consider degrees of relative squalor, it was also obvious that we had to develop very strong immune systems to defend against the many germy threats that undoubtedly existed even then (and maybe especially then). Even as recently as Medieval times, we have history books that chronicle outbreaks of plagues, cholera, typhus and the like, which most historians blame on poor hygiene habits.
Without electricity, our ancestors were largely at the mercy of the sun for light, and to hunt and gather, most would likely spend the bulk of their days out in the wind and sun (where we learned to “blink strong” - a habit that would serve us well when it came to producing oil from our eyelid oil glands). The “peasant diet” of fish, nuts and seeds also served to supply the essential “building blocks,” which would nourish those same oil-producing glands - so our ancestors were oil producing machines - well adapted to the harsh environments we habitated - even if our life spans were pathetically short in those hard times.
Fast-forward to the past 100 years and there has been a huge increase in our lifespan (I commonly see patients in their 80s-90s and some 100s, when the average prehistoric was apparently 20s-30s to be considered an old man or woman). Add to that, the benefit of a controlled environment - clean, well lit and with a temperature regulated by HVAC systems that can keep our room temperature as warm or cold as we wish - and “life is good.”
Digital devices keep us connected around the globe, providing access to education and entertainment that even the enlightened Leonardo Da Vinci might not have dreamed of. Food has become relatively plentiful for the average American, too. Unfortunately, the foods we crave today generally are weak in the oil “building blocks” our ancestors ate (their fish, nuts and seeds being a rich source of Omegas 3,6 and 9). Scientists claim we Americans eat 95% less of these “essential oils” in the last 100 years, thanks to “processed foods” like Pizza, Pasta, Hamburgers, Hot Dogs (sorry Joe) and all the chips and pretzels we munch while watching those athletes who train and perform in the sun and wind while we relax indoors on a comfortable couch or lounge chair (except for Joe). Staring at those digital devices trains the oil-producing glands not to work (where strong blinks are the triggers that make them work).
Finally, we turn to the issue of Rosacea. We all carry genes programed in our immune systems to fight germs and provide lethal forces to the surface of the eye when it is sending SOS-distress signals to our defense system. Some of us (with rosacea genes) are more “programed” than others to “fight the good fight” - even if that means interpreting mild, innocuous germs as “the enemy” and sending our defenses into high gear when they should be on idle. We “Rosaceans” (I may have just cloned that word?) will gradually develop ruddy red faces, thanks to the dilating blood vessels carrying those potent defenses. Eyes can get red (and dry), too. Was this a “survival mechanism” that allowed some of us to better subsist and ultimately procreate in those dirty caves, so we could launch the next generation? Tough to think of it that way, but maybe that was the genetic hack that was needed in those harsh times - and here we are today, paying another price in older ages than those forebears would have imagined. That price can be a form of dry eye disease where the oils we produce can be more like a pro-inflammatory “kerosene” (my euphemism for the harsh oils common to rosacea) than like the healthy meibum oils we would wish for in our tears. More on this and the treatments to help with this, in my future posting.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Rosacea and Dry Eyes Part 4 - why eye doctors get involved.
There is general agreement that Ocular Rosacea (OR) is common, under-recognized and under-treated. Yet the consequences of OR can be severe and sight threatening.
This article published a review of records from 131 patients who had Ocular Rosacea (OR) and were seen and treated by corneal specialists in referral practices (so not the average eye care clinic). Clearly some of these patients had been referred by general eye doctors because they had exhausted treatments they could offer locally - so this group of patients might be regarded as the “worst of the worst,” as opposed to the more average patients with more average/milder levels of eye diseases.
A “foreign body sensation” is also described as “a scratchy feeling” (like something got in the eye) and is perhaps one of the most common presenting complaints eye doctors see, along with burning (and, in pollen season, itching). Telangiectasias are the dilated, otherwise small blood vessels I described in the opening segment of ths series on Rosacea. Irregularities of the eyelid margin are common among those with chronic “blepharitis” (inflammation of the lids) and in those with a history of styes (which are also common in Rosacea patients). Meibomian Gland Dysfunction (or MGD) is an active cause of dry eye disease in up to 85% of sufferers - so while any one of these findings are beyond common to the majority of patients eye doctors see, the combination of these problems will most often indicate Ocular Rosacea. That 13 of these patients (or 10%) had compromised corneas which also compromised their vision is scary and even scarier is that six of these patients (roughly half) required corneal transplants (Penetrating Keratoplasty) in an attempt to restore their vision. Cicatrizing conjunctivitis is when there is scarring of the membrane over the white of the eye - which can lead to an inability to move the eye without causing pain and/or double vision and can lead to an inability to fully close the eye.
We will get into treatment strategies for Rosacea in general, and Ocular Rosacea in particular in future posts. Of note, is that some of the patients in this series were left legally blind and one lost their eye as an uncommon but frightful result of this disease. Since this disease affects both skin and eyes, it may require the combined skills and efforts of skin (dermatologists) and eye doctors (optometrists and ophthalmologists). It also requires eye doctors to “step back” and look at the whole face of their patients (and for skin doctors to also look at their patients eyes).
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
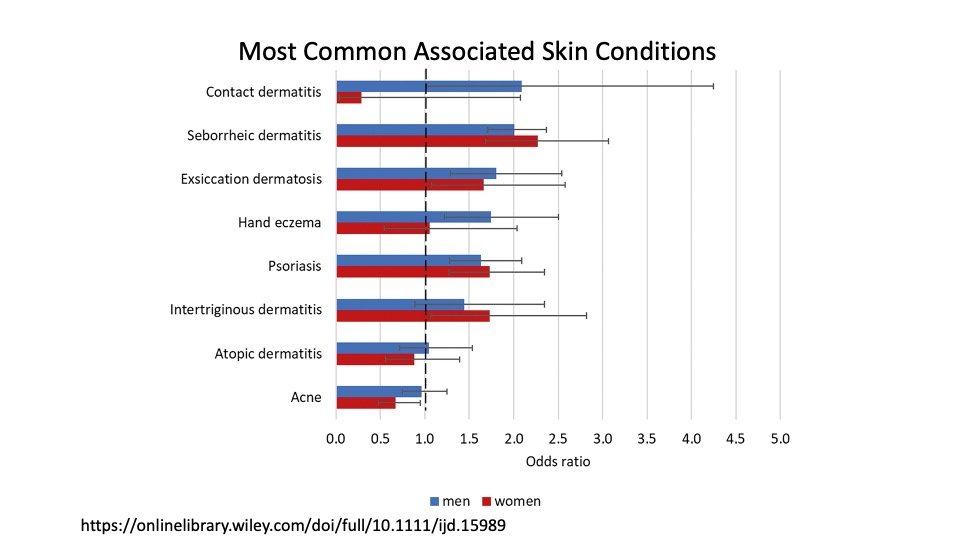
Rosacea and Dry Eyes Part 3 - Commonly Associated Skin Conditions
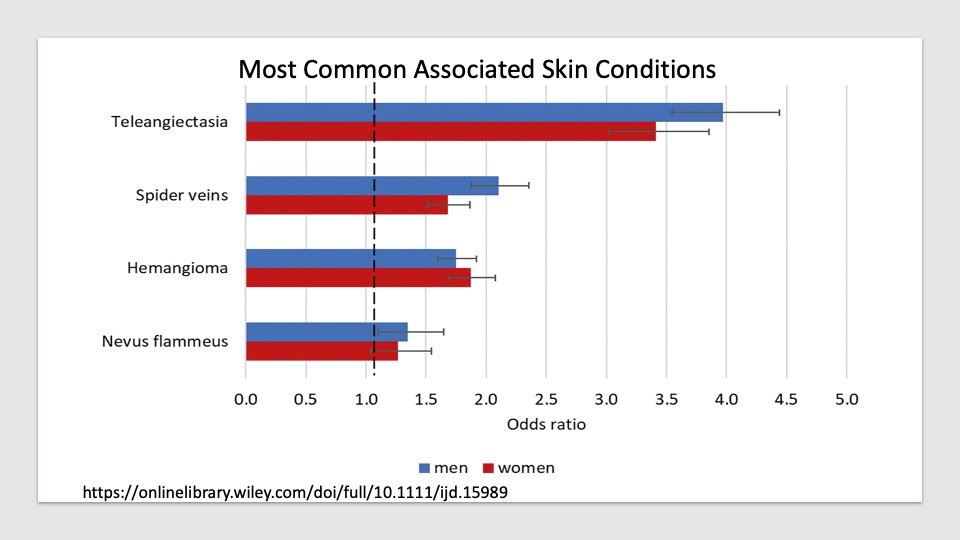
Telangiectasias are when tiny blood vessels called capillaries become dilated and occur 4 times more commonly in people with Rosacea. Spider veins are even larger dilated vessels and a hemangioma is a cluster of dilated vessels creating a small, red patch. Nevus Flammeus is another word for a “Port Wine Stain” - seen as a birthmark that looks like a “splash” of ruby red wine - and caused by a larger group of dilated blood vessels. In this study, men dominated the abnormal vessel frequency (except for the hemangiomas).
Rosacea is the genetic tendency for sensitive skin and irritable oil glands. I see these dilated blood vessels as a direct consequence of this sensitivity, though one could debate which came first, the dilated vessel or the sensitivity. Increasing blood flow will bring the immune system with it and thereby make skin more sensitive, even as the sensitivity can “call” more blood vessels up to the surface to bring the immune system to where it can act on whatever caused the sensitive reaction. (The old “which came first, the chicken or the egg.?” argument.)
Eczema is another word for sensitive skin and can come in as many as 7 different guises: https://nationaleczema.org/eczema/types-of-eczema/
Contact dermatitis is form of eczema causing a reaction of the skin to something that it comes into contact with (like the red, itchy blistery rash from poison ivy). Once skin is sensitized to something, anytime it comes in contact with “that thing,” it will react - typically more severely with subsequent contact.
https://www.mayoclinic.org/diseases-conditions/contact-dermatitis/symptoms-causes/syc-20352742#dialogId5001370
This is an excellent example from the Mayo Clinic, of patients I commonly see with contact dermatitis. They note:
Contact dermatitis on the face
Contact dermatitis often affects skin directly exposed to an offending substance. Here, the rash is likely caused by cosmetics.
https://www.medicalnewstoday.com/articles/seborrheic-dermatitis-vs-eczema
Seborrheic Dermatitis is another common form of eczema that is frequently seen in patients with rosacea. It tends to affect oily skin such as the face and scalp. This fellow’s lids are affected along with most of his face.
Each form of eczema requires its own type of treatment, and the area affected along with the degree of involvement will dictate the best treatment required. This will sometimes require the combined efforts of skin (Dermatologists) and eye specialists. In each case, if rosacea is an undercurrent, then that aspect should also be appropriately treated - along with any associated dry eye and related ocular surface diseases. More on this to come!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Rosacea and Dry Eyes Part 2 - How Common Is It?
Dall'Oglio F, Fusto C, Micali G. Intrafamilial Transmission of Rosacea Spanning Six Generations: A Retrospective Observational Study. J Clin Aesthet Dermatol. 2022 Feb;15(2):35-39. PMID: 35309876; PMCID: PMC8884184.
In this study spanning 6 generations of families related to patients with rosacea, there was a high familial association (which in this figure, shows how early in life - as in this grandfather, the disease can be minimally noticeable until much later in life). Further: “The results showed that 64 of 130 patients (49.2%) were positive for at least a family member with rosacea. In addition, 90 affected relatives (69.2%) were identified by extending the familial investigation to the whole kindred, finding a percentage of familiarity (69.2%) higher than that reported in the literature (30-50%) with a 1:1.4. ratio of patients positive for familiarity/affected relative.”
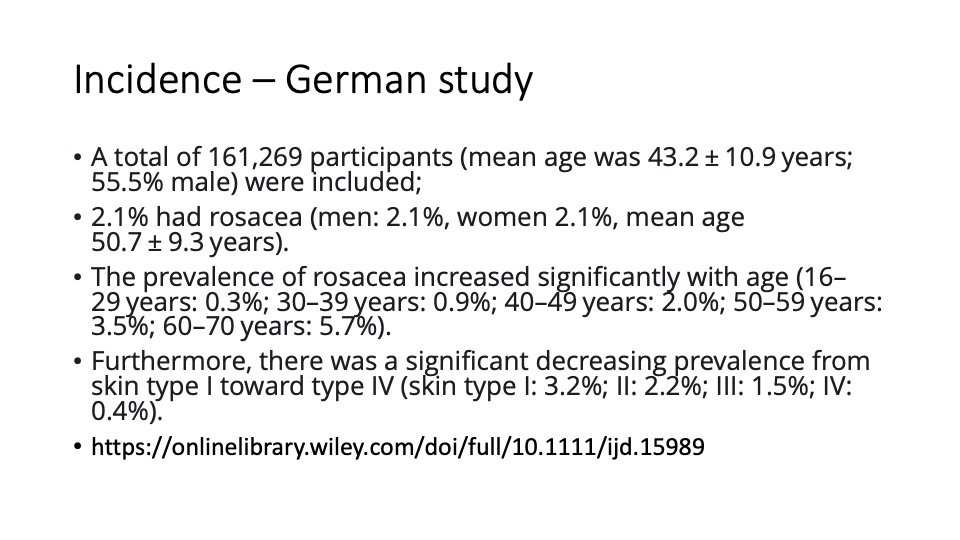
As a dry eye specialist, I tend to see a lot of Ocular Rosacea due to the common association with dry eye. Since all forms of Rosacea can have ocular-related components, I look closely at faces as well as lids and eyes, for signs of this disease. But just how common is Rosacea in the general population? According to a large German study which involved experienced Dermatologists doing the examination on over 161,000 employed German people from many kinds of jobs, the incidence was only 1 in 50 people, though it was closely tied to age - with those over 60 being the most affected (approaching 6%).
Yet when compared to a global analysis taking 26.5 million adults into consideration, the incidence appears closer to more than 1 in 20 people over 18 years old being affected. Interestingly, in my practice (heavily weighted to dry eye sufferers over 18 years of age), I’d say Ocular Rosacea (as determined with microscopic evaluation of the eyelids) is even more common than that. So what does this mean? Well, it really doesn’t matter how many people don’t have it, if you do. Fortunately there are good treatments for this and they work better when caught early and treated effectively.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Rosacea and Dry Eyes - a common pairing that needs recognition and treatment!
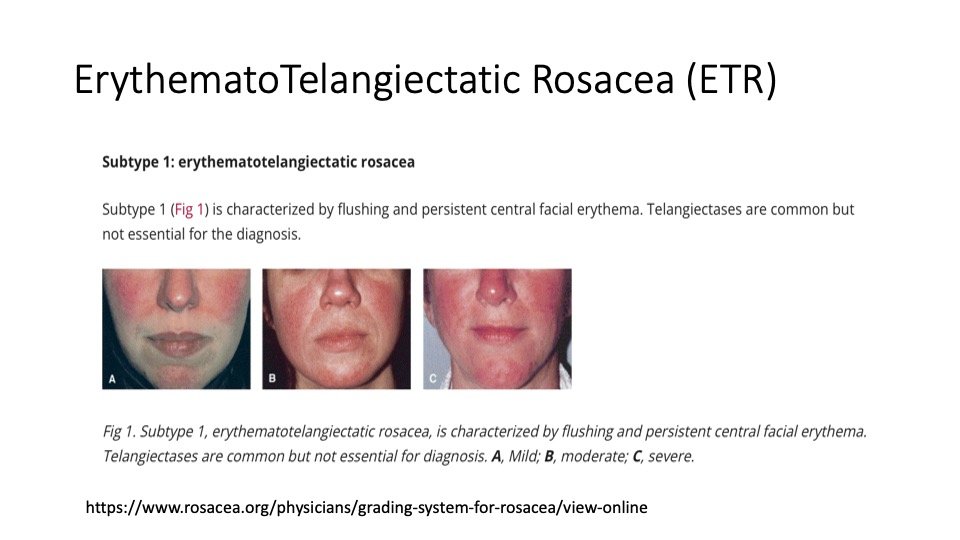
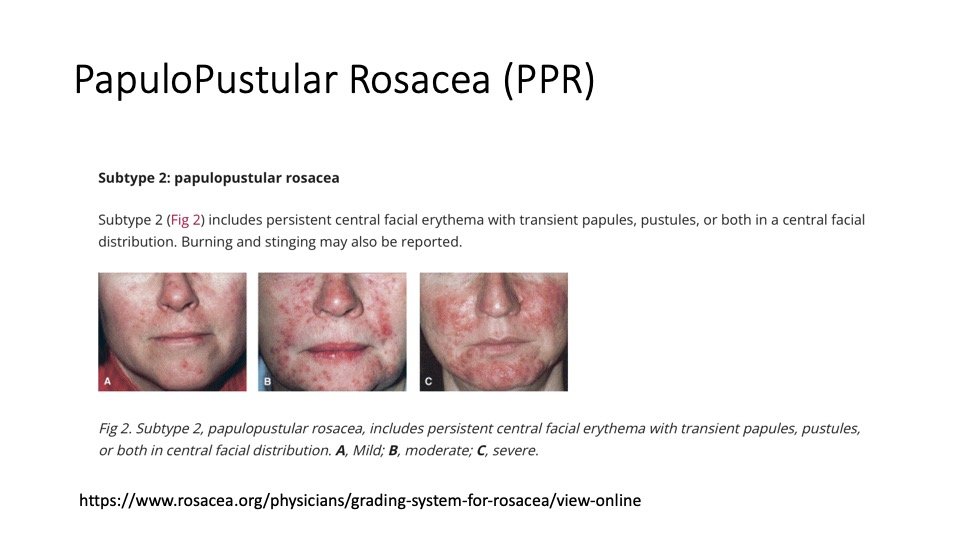
In simplest terms, Rosacea is sensitive skin and irritable oil glands. It commonly runs in families and is most obvious in those with pale skin but can affect any colored skin type (with darker skin harder to see the redness in, but can be no less affected than their pale-skinned friends). There are 4-subtypes and each can be graded from mild to severe (see my slides below). Because eyes are often affected - and eye doctors use microscopes to examine the eyelids and look closely at their patient’s faces, we frequently are the first to diagnose Rosacea (before their PCPs and often, even their Dermatologists do).
How Red is my face? ETR is all about the redness. Telangiectasias are the fine, red, “spider lines” caused by dilated superficial blood vessels. Less superficial vessels can dilate more broadly and give the general red hue to those affected.
“I’m too old for zits!” Papulopustular Rosacea fits the “Rosacea as Adult-Acne” theme. Papules are red bumps, and pustules are “white-headed zits.” Erythema is the undercurrent of facial redness like the ETR type listed above.
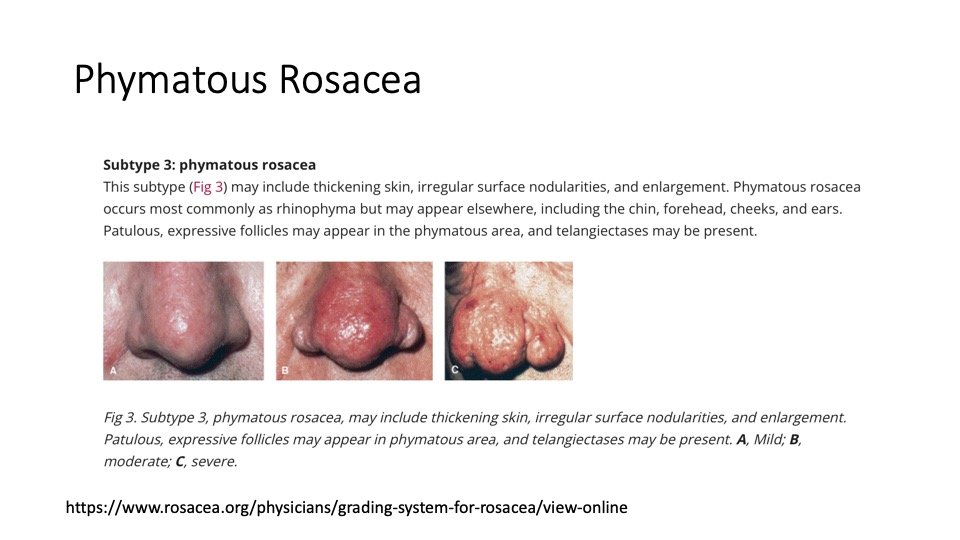
Why is my nose swelling up? Phymatous Rosacea is sometimes referred to as the W. C. Fields’ “Whiskey Nose,” but does not need alcohol to trigger it.. Even emotional flushing with the right genetic makeup can fuel it. Swollen vessels carry lots of blood and the thinner walls of the dilated vessels can leak clear blood-fluids rich in growth factors - acting like fertilizer to affected skin and making it grow thicker and bigger.
A common cause of chronic “red eye” (though there are many others) - most patients will have both eyes affected - but not always equally - and styes are common. This type can occur in conjunction with any of the above rosacea subtypes but can also occur by itself or before the other types become obvious. Once it affects the clear window of the eye called the cornea, severe damage can occur (typically, KERATITIS - a form of inflammation that can lead to scarring and loss of vision if central, or less commonly, ULCERS - a thinning and weakening of the cornea commonly related to infections that can lead to perforation and loss of the eye).
Since Rosacea can have devastating consequences for significantly affected eyes and eyelids, recognition is key as it should then lead to proper treatments. Even modestly affected eyes can have real - if not devastating consequences, I find most dry eye specialists to be uniquely suited to helping their patients with Rosacea - and future pasts will help to further explain the nature of Rosacea - the (good and bad) things that can affect it and some of the better treatments we can use to make it better.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
News Updates - more bad drops on the market and a new kind of “punctal plug” - Lacrifill!
First the bad news - FDA warnings about drops that could infect or injure you, continue:
”[1/31/2024] FDA is warning consumers not to purchase or use South Moon, Rebright or FivFivGo eye drops because of the potential risk of eye infection.
These are copycat eye drop products that consumers can easily mistake for Bausch + Lomb’s Lumify brand eye drops, an over-the-counter product approved for redness relief.” https://www.fda.gov/drugs/drug-safety-and-availability/fda-warns-consumers-contaminated-copycat-eye-drops?fbclid=IwAR085_VOsxm-9x0CtykAzUJF2Fb4Rn2nQzBFAd7HYsdwc6EBKu31z9hy_jI_aem_AfyHpReFyoRIaWRypfQKaucUi2WHDOhHkA7HxmLNfxqe1dwwFHXGJmlWgjMWkFb2a-A
I posted on Lumify (and other eye whiteners) - and the risks taken even with on-brand drops like these here: https://www.eyethera.com/blog/can-i-use-eye-whiteners-like-visine-or-lumify-when-my-eyes-get-red
Now the better news - and an update 4/14/25
April 7, 2024, I attended the American Society of Cataract and Refractive Surgery annual meeting. While I no longer perform cataract or refractive surgery, I see patients who have cataracts, and who may be planning cataract surgery, nearly every day in my clinical dry eye practice. I’ve posted on cataracts and dry eyes here: https://www.eyethera.com/blog/dry-eye-cataract-and-glaucoma-segment Control of the ocular surface is critical to a good outcome with cataract surgery, so I am often involved in the pre (and post) operative care of these patients. During that meeting, a new punctal plugging product. was rolled out, called “Lacrifill.” It is basically a sugar gel like “Juvederm” or “Restylane” (a natural “hyaluronic acid” compound found in skin and eyes) that has long been used as a filler in cosmetic procedures and in cataract surgery. It will gradually dissolve into sugar and water, so needs replacement approximately every 6 months (& may last a bit longer - or less long, for some). If it works “too well” and results in chronic, unwanted tearing (down the cheeks), then a salt water solution can be used to rinse it down the “plumbing” into the nose. There is also an enzyme that can dissolve it in cases that a simple rinsing doesn’t work (expected to be rare). Insurance is expected to cover it (and as of April, 2025, it has been getting covered by most medical insurance companies), as a plugging procedure, but it’s possible that some may require a “prior authorization” approval process. Punctal plugging is not for everyone (I’ve blogged about this before: https://www.eyethera.com/blog/what-about-punctal-plugs-or-why-not-dam-up-those-damn-tears and https://www.eyethera.com/blog/when-tears-dont-drain-properly-you-get-toxic-soup-and-the-toxic-soup-syndrome
While these prior posts cover most of the potential “negatives” involved with blocking the normal flow of tears from the eye to the nose, it is true that there are numbers of patients who will significantly benefit from such tear duct closure. Keeping more tears (and any medicated products) on the surface of the eyes is hepful when the tears are “good tears” but just too little to do their job. A potential benefit of this unique use of sugar gel, is the “soft” and “sticky” quality of this natural filler. This means no “plastic” is exposed to the delicate membranes of the eye, and nothing to “fall out,” which is a common problem with the plastic plugs that are “wedged” into the tiny tear duct openings along the inner eyelid margins. Lacrifill can “hug” the passageways leading from the eyelid to the nose, blocking tears along the entire way.
A few key points - as a sugar gel, the reason it doesn’t instantly “dissolve” into sugar and water, is due to the “crosslinking” where the sugar molecules are bound strongly to each other. Natural enzymes break these links down over time and the more “links” in the chain, the harder it is to break down. Staying soft and “gel-like” means that excessive manipulation (squeezing, massaging, rubbing) may cause some gel to “burp out” of the tear duct (either into your tears, or down your nose), so avoidance of excess manipulation near the tear drainage area should generally be avoided with this product (especially in the first days of instillation, as most sugar gels tend to “set up” and become more locked in place as they mature in their position). If too much burps out and into your tears, this leaves a portion of the duct “empty” with a blockage in place closer to the nose. Typically, this can lead to a “stagnant pool” of tears where germs can thrive and potentially cause infections. If the area of the lids closer to the nose become infected, then sticky yellow-to-greenish discharge and/or redness, swelling, tenderness and warmth of that area can indicate an urgent need to see your eye doctor. I can share that one year into these treatments, I have yet to see any infections I would blame on this product.
As of April 2025, I can add that I have used this product extensively and have found no significant side effects over the past year. One patient felt a level of discomfort on one side of her face which she felt likely related to the product - so had it removed. However upon removal (flushing out), she felt the same discomfort and ultimately requested more Lacrifill be placed into the area that had been flushed out, to replace it (as, in retrospect, it appeared to have significantly helped her Aqueous Tear Deficiency). I have had to “top up” a few patients prior to the 6 month expectation. Because we can chose (as I and my patients most often do) to place the Lacrifill into the lower tear drainage system (and leave the upper drainage intact), the residual intact passage can allow some reduced turnover of the tears. This prevents the “Toxic Soup” issues I’ve posted on - but I have had a few patients who have had full plugging of both upper and lower systems and have yet to have a complaint about excess tearing (usually because the Aqueous Tear Deficiency was that severe).
I do advise that there can be several days (3-5 are typical) where the reflex tearing (what I call the “fire hose”) can remain overly active (as it may have had to be to keep up with the poor output of the “sprinkler system” of so called basal tear production). This can mean more actively tearing for those initial days (until the fire hose gets the message that it is no longer required so much), but this generally settles down after those 3-5 days. Lid hygiene remains critical (and even more so than usual) once punctal plugging has occurred - as the toxic residue from eyelid germs (and sometimes from toxic eyelid makeup) can “stew” on the eye’s surface and cause more inflammation and irritation.
As usual, I recommend working with a dry eye specialist to get the best results for your dry eyes.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Making Tears Part 8 - More on Making Proteins…
A couple of posts ago, I referred to the intricate “bakeries” inside the castle walls (which I count as the Lacrimal Gland), where production of proteins like “Sir Lact,” “Sir Lyse” and a whole army of defensive “Knights” occur to keep the realm (the eye) safe. Outside the castle, there are the “rolling fields” of conjunctiva (the smooth, clear membrane covering the whites of the eyes) as well as the cornea (the window or “watch glass” we see through). Among that membrane field are tiny cells I referred to as the “Peasants” working that field. Served by blood vessels carrying proteins and other nourishing products, these Peasants (called Goblet cells”) can “belch out” a special, sticky protein, called mucus. Their distribution is not evenly spread across the landscape, but the “mixing action” of a blink can help distribute their sticky products over the surface of that realm. Because the surface would be very slippery without this “peanut butter-like substance” to help adhere, a key attribute of this product is the very sticky nature that interacts with the salt-watery tears floating above that layer and allows it to spread its goodness while acting as another barrier to any “badness” that would like to attack that surface. As sticky as it is to the cells below the tears, it has unique properties that makes it hard for germs to get to - and stick to - that surface!
The nose-favored distribution of the “Protein Factories” called “Goblet Cells.” (tiny dots are the cells with some clusters as larger dots. N stands for Nose).
From: Gipson IK. Goblet cells of the conjunctiva: A review of recent findings. Prog Retin Eye Res. 2016 Sep;54:49-63. doi: 10.1016/j.preteyeres.2016.04.005. Epub 2016 Apr 16. PMID: 27091323; PMCID: PMC4992623.
The Calcium “tokens” play a role in switching on the production of that sticky protein and the hormone messenger, Vitamin D, has receptors that it can bind to, and help in increasing the supply of Calcium - which can initiate greater protein production. Vitamin D has come under great medical interest, as it has similar mediating roles around the entire body - and the deficiencies of Vitamin D common to many of us in the North East, means many of my dry eye patients are at a disadvantage, since natural sources of Vitamin D come from exposure of the skin to the sun, and in this area winters are long, winter days are short and often cloudy. Primary care doctors are increasingly tuned in to monitoring Vitamin D levels and often recommend Vitamin D3 supplements. Cod liver oil, a prime source of Omega 3, is also a good source of Vitamin D and it is part of the supplements I recommend to most of my patients. Around the “mouth” of these goblet cells is a “belt-like” band that can help regulate the “belching,” by adjusting the size of the opening that would allow the proteins to escape (a bit like a chimney flue that regulates the escape of smoke from a fireplace). As the concentrated protein escapes, it mixes with water and “blooms” into the sticky paste we call mucin or mucus.
But Goblet cells are not just “protein factories,” indeed they appear responsible for the water expressed from the conjunctiva itself. Using my “sprinkler and fire hose” analogy, the Goblet cells produce “Claudins” a type of chemical “worker” that can open little water channels in the membranes of the Goblet cells and help regulate their “sprinkler function.” The Lacrimal Gland is the primary source for the dousing of salty water I refer to as the “fire hose” - so that water can really flow when it is most needed.
Production of these important Goblet cells, comes from unique stem cells - different but related to the stem cells that cover our corneas with their specialized cells. They have an interesting biological clock that produces crops of these “peasants” based on a cell-doubling calendar. Most of the time they crank out epithelial cells - the tough “tiles” that make up the resilient cover of our membrane, but at regular intervals, they switch gears to produce the Goblet cells! Inflammation appears to affect production of these Goblet cells - and allergies, infections and self-induced irritation (as in Mucus Fishing) are well known factors in increasing their protein production - see my post on this here: https://www.eyethera.com/blog/when-eyelids-are-irritated-including-allergies-such-as-to-our-best-friend-pets
Not all proteins produced by Goblet cells are the sticky things outlined above - some have additional sugar complexes that make them uniquely suited to assist in repair of the corneal surface (think of them as the medical emissaries or local “Red Cross” if such a thing existed in our Medieval world). Genetic tweaks in the production of similar Goblet cell proteins can lead to a real world autoimmune disease - Ocular Cicatricial Pemphigoid (OCP - mentioned in my autoimmune posting - now called “mucous membrane pemphigoid” - see the next link, below), where the surface progressively scars and can lead to exceptionally dry surfaces that can result in blindness for those not sufficiently diagnosed and treated.
Cyclosporine (medications like Restasis, among others) has anti-inflammatory properties that can lead to as much as a 2-fold increase in the number of Goblet cells (by reducing the inflammation that reduced that number), as well as an increased water production (and overall “sprinkler system” tear volume) for our tears. This appears relatively unique among anti-inflammatory medications and may be especially helpful for those patients suffering from reduced mucin (common to those with significantly advanced dry eye disease called “Aqueous Tear Deficiency” - see my prior posts on water, including: https://www.eyethera.com/blog/when-the-sprinkler-system-dries-up-and-autoimmune-testing-is-negative-whats-up ). Vitamin A also plays a role and while we know too much Vitamin A has been associated with MGD (Accutane for one), some amount is needed for proper Goblet cell development and activity. In fact, the brain-eye “axis” development is heavily dependent on Vitamin A from conception. Because Vitamin A can be produced as needed from a diet rich in leafy green vegetables, this appears yet one more reason to include these foods in your diet!
Many diseases wage war on Goblet cells - allergies, Autoimmune diseases (i.e. Stevens Johnson Syndrome, OCP, Sjogren’s, Graft vs Host) as well as advanced dry eye disease, radiation and even blepharitis (see my many posts on that issue). Keeping Goblet cells healthy is one more goal for dry eye doctors to have for their patients - those poor little Peasants are no less noble than the Knights, Kings and Queens, when it comes to keeping a healthy, happy realm.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Making Tears Part 7 (the all-so-important oil glands!)
While there is no debate that water, salts and proteins are principle portions of the tears, it is the fine layer of oil floating on top, that seals in that moisture and lubricates - while supporting and protecting the eye. The production of oil involves a complex cycle of life from “mother cells” (called “stem cells”) who produce “daughter cells” (called “progenitor cells”) that in turn birth “oil cells” (called “meibocytes”). Mother cells exist near the surface of the lid margin and along the “tunnels” (ductules) leading to the “chambers” (acini - the “balloon-like” “rooms” off these passageways). Their progeny or daughter cells can migrate into these chambers and produce the oil cells or meibocytes, where they “hatch” into little puddles of oil.
While this sounds surreal, simply because it is a complex process, one can understand that there can be many pitfalls which can weaken the “supply chain” otherwise leading to this oil production. Add that it is necessary for the force of a blink to “flush out” and empty these chambers - and we begin to see the kind of trouble leading to “Meibomian Gland Dysfunction” (or MGD). I’ve posted much on the basics -the importance of oil and its production, as well as various tactics to improve oil production, in earlier blog posts: https://www.eyethera.com/blog/how-important-is-oil-to-our-tears , https://www.eyethera.com/blog/how-do-we-fix-the-oil-problem, https://www.eyethera.com/blog/you-are-what-you-eat, https://www.eyethera.com/blog/why-do-my-oil-supplements-not-work , https://www.eyethera.com/blog/why-do-expensive-dry-eye-treatments-fail-and-what-is-maskin-probing , https://www.eyethera.com/blog/more-on-mgs-the-tear-oil-glands , but to distill it down to the present level of discussion, I can add a few extra thoughts.
Remember the “peasant diet?” Fish, nuts and seeds, whole grains, and legumes - not only supply Tryptophan, leading to Serotonin and Melatonin (see earlier posts in this series), but also provide the (3) Essential Free Fatty Acids - the “oil building blocks” called Omega 3, 6 & 9. Without a steady supply of these essential oils in our diet, the mother and daughter cells making the oil cells are just as hampered as a mother trying to birth a healthy baby when they are malnourished. Toxins (potentially from pollution, makeup, medications like Accutane or other retinoids - or from germ warfare on our lid margins, among other stresses) can weaken and kill off these maternal cells. Inflammation can undermine the foundation of the walls supporting the tunnels and chambers, leading to strictures and “dead ends” that can block the passageways required for flushing out the oils produced in those chambers. Too much inflammation can weaken our troops and act like a fire that can burn down the village.
When oil doesn’t move along as it should - it becomes stagnant, rancid, nasty stuff that by degree tends to “gel up” and turn into the kind of waxy products better suited for making candles than it is for making tears. Once the lids become aware of just how bad the oil has become, it senses it as the “enemy” and inflammation will attempt to wall it off. From what I read about sanitation in the Middle Ages, walling off unsanitary stuff was about all they could do when modern plumbing didn’t exist - so maybe our lids aren’t all that different? Unfortunately, this can lead to our inadvertently damaging these oil producing glands. Caught early, it is often easy to “fix” this problem - but when allowed to progress, then styes and withering are the common outcomes - followed by ever decreasing amounts of oil production. I’ll direct readers to the above links for more clinical information on these topics and look deeper into the protein factories called “Goblet Cells” next time.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Making Tears Part 6
Regulation is the key to running an efficient, effective realm, no matter what era or place is involved. In the case of dry eye disease, this is especially true, as this is where regulation has often gone amiss of our healthy aim. Cortisol (a messenger from the adrenal glands) is responsible for helping us in coping with stress. I see it as the emissary sent to warn of an impending enemy “siege,” and sets in motion the ability to free up energy and promote the “S” camp to “protect the realm” from the “attacking Huns,” with its emergency rations and protective reflexes. The problem is that we can only stay on this level of “high alert” for so long, before we begin to literally “break down.” This is another way of saying that reducing stress levels and the cortisol levels related to it, is important for restoring “normalcy” to the daily functions of the castle and protect the general health of its populace. Other ways we raise our cortisol levels is with alcohol. As little as 2 ounces of alcohol can raise this level and set us on this “S” pathway for days. Illness will also activate cortisol production, so staying physically healthy is key to eye health as well as general health. (Often easier said than done.)
Caffeine is a powerful “S” camp activator as well. It sends a message to prepare for “Flight or Fright,” where our heart rate, blood pressure and breathing rate is increased. This may help us prepare for our often stressful days ahead, but does take some toll on the tear glands and the surface of our now “saltwater -rather-than-salad-dressing-drenched” eyes. While we may not be able to easily regulate the amount of stress in our day, we can regulate the amount of caffeine and alcohol we take in. Both can adversely affect sleep, so caffeine is best consumed early in the day and alcohol in moderate amounts early in the evening. For those suffering significantly from dry eye disease, avoiding all forms of caffeine and alcohol can often be a game changing strategy.
Sleep and rest are the gifts that elevate the “PS” camp activities that restore the “salad dressing” and replenish the stores of healthy tear products that were "burned up” by the “S” camp. Melatonin is the “sleep hormone” that sets sleep in motion and can be promoted by “winding down” from online and TV/computer/gaming and phone/online activities a few hours before bedtime. I posted on issues relating to sleep here: https://www.eyethera.com/blog/do-blue-blocking-glasses-help-with-dry-eyes - and relative to the “peasant diet” as it can affect sleep, here: https://www.eyethera.com/blog/making-tears-part-2
Inside the cells lining the inner eyelids and white part of our eyes, live “protein factories.” Inside these “castle rooms",” coded messages (Messenger or “mRNA”) work with the protein architects (called ribosomes, I think of them as “bakers” and the “recipe” comes in the form of mRNA). The baker collects the necessary ingredients and then mixes them together in the “mixing bowl” called the Endoplasmic Reticulum (ER). This gets passed along by way of “chaperones” into the “oven” called the Golgi Apparatus (GA). Once “baked” into the form required by the recipe, little “sacs” can pass them through the “wall” of the cell membrane and release the final product into the water seeping through the same membranes. Again, the “salty tokens” help regulate this exchange and are driven by programmed codes that help regulate all cell life.
Salts can be similarly stored and passed through the membranes, to join the protein-laden water. At this point, we have the water, salt and protein forming the essential 3 parts of our “tear salad dressing,” but to get to the ultimate tear, we need to add oil. We also have signals in the way of nerves and hormones to regulate the volume and ultimate recipe of our tears. In future posts, I’ll attempt to explain more of this interesting and essential process. I can also share that eyes prone to repeated infections may have some difficulties in producing “Sir Lyse and Sir Lact.” Others may lack some of the antibodies and other protective mechanisms common to most people. Science continues to “drill down” on these deficiencies and continues to look for remedies.
One example of this “Better living through chemistry” act, is understanding - and modifying - our protein messengers. G-proteins are important Medieval “Pages” - messengers that couple with cells at the “in box” to affect the activities of the cell. In a remote region of the realm (the brain’s hypothalamus) these messengers can be dispatched to circulate throughout the “aqueducts” (blood vessels) and reach the targeted tissues (in our case, the tear producing “machinery”). OKYO Pharma has apparently capitalized on one of these “Pages” (for a fuller scientific account, see: https://okyopharma.com/okyo-pharma-announces-ok-101-successfully-achieved-statistical-significance-for-multiple-signs-and-symptoms-of-dry-eye-disease-including-ocular-pain-relief-in-its-first-in-human-phase-2-trial-of-ok-10/ - A quote from this article about the drug they’ve named OK-101, explains it succinctly: “OK-101 is a lipid conjugated chemerin peptide agonist of the ChemR23-protein coupled receptor which is typically found on immune cells of the eye responsible for the inflammatory response. OK-101 was developed using a membrane-anchored-peptide technology to produce a novel long-acting drug candidate for treating dry eye disease. OK-101 has been shown to produce anti-inflammatory and pain-reducing efficacy signals in mouse models of dry eye disease and corneal neuropathic pain (NCP), respectively” and Okyo Pharma “announces additional statistically significant findings in results from Phase 2 trial of OK-101 (0.05%)” - so by making a drug mimicking a G-protein “Page” we now may have a way to target the “Knights” who may have gone too “rogue” and would otherwise cause inflammation-related mayhem in corneal nerves and tear gland tissues. Understanding the cellular level of how our bodies work can allow science to help put our bodies (and eyes) back on a peaceful track and improve the quality of our lives.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Making Tears Part 5
In previous sections of this series, we’ve learned about some of the many proteins and salts making up our tears - but we have yet to discuss where (and how) we get the water. It should be obvious that every element of our tears ultimately comes from our diet and digestion (and the many, tiny germs relevant to that digestion process) - and no surprise that the water comes through our gut as well. I’ve covered much of this in prior posts, but how do the tiny cells in our lacrimal gland and scattered over the smooth membranes covering portions of the eye and eyelids ultimately regulate and produce that water? Remarkably, scientists continue to be befuddled by this process, but much has been learned from studies (largely using rodents). I’ll use some artistic license around my medieval analogies to help explain what I know about this interesting process.
Remember those salty “tokens” we called sodium and calcium “ions?” These tiny, “charged particles” have an electrical nature which allows them to bind and then “flip switches” in cells. Pathways open, allowing materials like water to pass through otherwise watertight membranes - and water likes to follow these ions - so cellular “pumps” can be triggered and run by these tiny tokens. Scientists refer to this production of water as “transepithelial” - indicating that the water literally passes through these (epithelial) cells and around or through the binding agents acting as the “mortar” between these cells. Of equal interest is that there are “protein factories” inside these cells that make the products (like Lactoferrin and Lysozyme) which can be transported into the water that becomes our tears.
Flow is a highly regulated process involving the “telegraph wires” (a neural network), as well as local and distant messengers (proteins and hormones). Some merely open or close the “aqueducts” (blood supply), so more water is delivered to the tissues. The “S and PS camps” (Sympathetic and Parasympathetic Systems) are good at this part of the regulation and many drugs have activities in this realm. A good online source for finding medications related to the “S” camp can be found here: https://go.drugbank.com/categories/DBCAT000438 but the effects are complex, as these messengers not only increase circulation, but also may stimulate muscles which open lids further (those knights on horses pulling the carriage around), which will expose the eyes to evaporation (and drying out). The “S” camp is also primarily responsible for the “fire hose” or emergency backup system making the salty tears we actively cry with (the buckets of fire-prevention water we make when sad, when something gets in our eyes or when the sprinklers let us down). The “PS” camp has an equal resource here: https://go.drugbank.com/categories/DBCAT000448 and is generally responsible for the "“sprinkler system” making the “salad dressing” of a healthy tear.
It is not uncommon for me to find dry eye patients on dozens of medications, treating a wide range of symptoms and maladies. Some of these drugs are countering side effects of one another, which can relate to these 2 opposing “camps.” Sorting out which medications are truly necessary - and weeding out those that are less necessary (or only used as counters to side effects that disappear when those medications are weeded out) often requires input from the various doctors who prescribed them - so it can take a literal “village” to help an average dry eye patient. Our eyes, like our bodies, are a complex chemical factory, with all the general issues for successful survival and flourishing, as those “medieval realms” - adequate nourishment, rest, support, protection and order. Without proper elements of each, chaos and “plagues” can take us down. More on this internal and external regulation next time!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Making Tears Part 4
Ah, Sir Lyse. Lysozyme is an enzyme that dissolves the sugary protection around bacteria and causes them to dissolve or “lyse.” I think of that sugary protection as a kind of chainmail mantle, since it is designed to allow some bacterial needs in and bacterial bad things out - but otherwise protect like a chainmail mesh can do. This mesh is the foundation of the bacterial cell wall, the protective envelope those wicked little assassins have as their best defense. Like the wicked witch in the Wizard of Oz, once the protective “spell” of this chainmail is lost, the bacteria is “melted” - like pouring a bucket of water did to her. As you can see from the table below, tears contain the greatest amount of “Sir Lyse” compared to many other natural sources.
Table 1 (from Nawaz N, Wen S, Wang F, Nawaz S, Raza J, Iftikhar M, Usman M. Lysozyme and Its Application as Antibacterial Agent in Food Industry. Molecules. 2022 Sep 24;27(19):6305. doi: 10.3390/molecules27196305. PMID: 36234848; PMCID: PMC9572377.Selected sources of lysozyme.)
Source of Lysozyme Amount of Lysozyme
Tears 3000–5000 µg/mL
Chicken egg white 2500–3500 µg/mL
Duck egg white 1000–1300 µg/mL
Goose egg white 500–700 µg/mL
Human milk 55-75 µg/mL
Cow milk 10–15 µg/mL
Cauliflower juice 25–28 µg/mL
Cabbage juice 7–8 µg/mL
Papaya juice 9 µg/mL
Spleen 50–160 mg/kg
Thymus 60–80 mg/kg
Pancreas 20–35 mg/kg
According to this same article, “Lysozyme is an important part of the innate immune system and exhibits strong antimicrobial activities against bacterial, fungal, and viral pathogens. It protects against infections, acts as a natural antibiotic, and enhances the efficacy of other antibiotics, while it also strengthens the immune system.” This sounds a bit like Sir Lact (Lactoferrin) - and helps us understand how, when mankind was living in dirty caves and hovels, we (through this roundtable of shining knights) were able to sustain ourselves against the many diseases that would otherwise have wiped us out. (Interesting that even plants like cabbages and cauliflowers can contain some amount of Sir Lyse - and how, at some basic biological level, our tears reflect eons of evolution that. even include the plants we also survive on).
Further, “The protein was suggested to conduce to the destruction of tumors, as it modulates the synthesis of the tumor necrosis factor (TNFα) and also stimulates the production of Type I interferon (INFα, INFβ, INFγ), interleukin-2 (II-2) and interleukin-6 (IL-6) by human lymphocytes [7]. In the current pandemic of the coronavirus, some modified form of lysozyme can be used to stimulate the formation of interferon, an effective substance against coronavirus, and thus reduce the risk of the life-threatening form of COVID-19 up to 79% [8,9].”
Apart from Sir Lyse, Sir Lacto and our antibodies, we have other “protectors of the realm,” including tear-specific prealbumin (TSP or lipocalin) and peroxidase. Add to that the natural “washing function” of blinking away old, dirty tears and replacing them with fresh, healthy tears and we have a robust defense system. Even as pathogens evolve to take us down by “getting smarter and better armed” - so we too can rely on our defenses to evolve - and, with modifications, keep up with these tiny infidels, assassins and assorted mercenary troops. Eyes are precious and it’s good to know we can protect them with our tears (and with our strides in science that allow us to create medicines, vaccines and strategies that can aid our innate defenses).
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Making Tears Part 3
For those interested in the relationship between sleep, diet and health (and don’t mind some technical talk), this is a good place to start: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8511346/#:~:text=Tryptophan%20is%20an%20essential%20amino,and%20legumes%20(Table%201).
Getting back to the basics of a tear, this “salad dressing” consists of surface “oils,” a mid-layer of salty water and an inner layer of proteins described as the mucus layer. While each element has specific functions - the primary functions involve transporting oxygen to the surface cells (this is where the salty water plays a critical role) as well as protecting and otherwise supporting them. The oil is a thin “slick” produced by the Meibomian Glands - which are “accordions” in the eyelids and are literally pressed into service by the squeezing pressure of a “good blink.” We will delve deeper into this part of the tear-making discussion later and refocus on the salty water and proteins, here.
If we can use simpler measures of volume to describe a tear (normally measured in microns), then 1-2 “ounces” of the recipe is oil, 7-8 “ounces” is the salty water and as much as 30 “ounces” is the protein “mash” (proteins and sugar complexes suspended in water) we can call mucus. Spread across the surface with a blink, this is the support needed by the “peasant” surface cells and needs to be sustained regardless of the environment (however cold, hot, dry or humid those conditions might be). Treachery in the way of infectious invaders, surface scratches (where a fingernail could be the equivalent of slings and arrows) or siege (the effect of too much staring - so the supply of fresh tears is interrupted and the peasants “go without”) will call on support from within and without the castle walls.
When various messengers (there are many, but include Acetylcholine or ACh and Vasoactive Intestinal Polypeptide or VIP) arrive by way of the major roadways (in our case, nerves and blood vessels), they’re received by their own, external messengers (G-proteins) and make their way to the cell “factories” making the protein products and regulating the transfer of water - largely regulated by Calcium ions (the salty tokens that open these cellular pathways). Other proteins like Immunoglobulins (IgA) are produced by specialized “plasma cells” that can arrive from the gut by way of the blood vessel roadway and can sit amongst the Lacrimal Glands “normal” cells. This appears to be a pathway for the “Gut Associated Lymphoid Tissue” (or “GALT”) to bring immune functions learned from interaction with gut germs to bear on eye protection - but may also open the door to malfunctions leading to autoimmunity (where they become traitorous and inflict damage on normal cells instead of abnormal invaders).
When it comes to fighting germs, protection from “within” comes from a number of “on site” agents. We would get deep into the weeds if I attempt to single out and discuss each one, but there are a few that deserve significant attention here. I’ll begin with Lactoferrin - I see this as an exceptional band of knights who are present in tears and throughout the body - more heavily present in the smooth, moist membranes where germs are likely to first approach us. I’ll refer to this element as “Sir Lact” (yes - lac or lact is derived from the latin word for mik and Lactoferrin is highly present in milk - probably to ensure the offspring being sustained on that milk will have an extra opportunity to fend off infections until they can mount their own vigorous defense system). Sir Lact has the ability to bind iron (so essentially cloaking himself/herself in armor, while denying his foe the same). Iron is critical to bacterial survival and Sir Lact can not only deny them their iron, but also directly damage the membranes of these microbial foes - while signaling other members of our defense system to attack. Interestingly, Sir Lact also helps to control cellular oxidation (think of this as “biological rusting” - and this process of oxidation puts stresses on cells (good or bad) and controlling inflammatory responses - so controlling these processes may help us “age slower,” as well as helping us deal with some of the root causes involved with many neurological diseases (Parkinson’s and Alzheimer’s, to name two), many autoimmune diseases (like Sjogren’s and Rheumatoid Arthritis, to name two more) and cancers (too many to name). Sir Lact appears effective against many bacteria (including some who would be resistant to many of our modern-day antibiotics) and also many viruses. He/She can potentially fend off attackers so we have more time to recognize them and call in specific antibodies and other immune responses that can be more specifically directed to kill those foes. Sir Lact works well with other members of a tear’s defenses, including “Sir Lyse,” (Lysozyme) who will be heavily featured next time.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Making Tears Part 2
When visiting Poland a number of years ago, I had a chance to experience their renowned salt mines and - by visiting some museums and a castle, to gain an appreciation for what it meant to be royalty in the Middle Ages. (If any of you get the chance, I’d highly recommend a tour there.) This creates the next level of our discussion, as salt was a form of currency - so important and highly sought after as it was - and so critical to the production of our tears! For a detailed history of the salt mines, I recommend:
First, not all salts are Sodium (what we commonly think of as table salt) - and Calcium (another common salt vital to our lives) plays an important role in tear production. Calcium ions can be seen as tokens that open gates across membranes (I liken them to the gates in the cell or “establishment” walls that allow movement in and out of that establishment). Sodium also plays an important role and can “carry” the water in and out of the cells.
Regulation of these establishment activities (producing the salt-watery part of the tears) occurs from two “camps” - (Sympathetic and ParaSympathetic - we’ll establish them as the S and PS camps). Acetylcholine (ACh) is the messenger of the PS camp and generally tells the establishments within the larger castle (Lacrimal Gland) what to do regarding the basic, daily tasks of tear production (how many buckets of salty water are needed to sustain the surface of the eye - perhaps we can see those surface cells as the peasants). This establishes the daily rations - but is heavily influenced by the S camp (which communicates by epinephrine as well as a host of other hormones/transmitters). The “flight or fright” response of the S camp is the call-to-action responsible for emotional and reactive or “reflex” crying and can substantially increase the volume of rations (which has the benefit of washing away damaging irritants, apart from social responses).
Many of the finer aspects of hormonal influences remain poorly understood, possibly because there are too many “voices” at the table at any given time. The “Feudal Lord” ruling the Lacrimal Gland “castle” has many “advisors” (known as the biological “receptors” - or, in this analogy, the “ears” of these advisors). They get their messages from the many hormones and transmitters sent directly from the "King or Queen” as well as less directly, from the many hormone centers throughout our bodies.
One hormone called Serotonin appears to play a pivotal role in tear production (based on mouse research). Serotonin is best produced by a diet rich in Tryptophan, which is an essential amino acid found mostly in animal products, as well as in nuts and seeds, whole grains, and legumes. This “peasant diet” - good for producing Tryptophan - contributes to production of Melatonin - the sleep hormone - and since sleep appears to be linked to health in general and to production of healthy tears in particular (in this conversation), it is easy to begin seeing the underlying links to this happy “Medieval life.” (We will circle back to the essential Omega Oils found in fish, nuts and seeds when we get to the Meibomian Glands and their oils).
We’ll delve into more of that “Round Table” discussion next time.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Making Tears Part 1
To learn how tears are made, it is helpful to understand the elements in a tear, as well as the hierarchy of signaling and basic arrangement of glands and tissues required. for that production Most will appreciate how the brain is the key regulator - King (or Queen) to their servants, including, in this analogy, the organs and glands that define our bodily actions.
Nerves serve as the telegraph lines (yes, telegraphs came much later in the scope of history, but it’s hard to imagine faster lines of communication in the medieval era), communicating these royal wishes to their servant subjects, In turn, these subjects send back their sensations - as reports and needs - by an alternate series of telegraph lines, so the Royals can serve and sense what’s going on around them. Apart from all this commotion, exists the most basic daily activities, including the making of tears. Furthering my medieval analogies, this would be the regulation of Peasants and more lowly Serfs, by Knights and their Lords.
I see each eye as a Lord, served by Knights (on horseback;) - acting as the muscles to move their Lords around in their carriages, (the orbit). Other Knights (with their own set of Serfs) exist to clean, nourish and protect them. Eyelid Knights are supported - outside - by skin and eyelashes (to shield from the elements) and are supported inside - by membranes, glands, and plumbing to make and distribute tears). Over all of this, a Round Table of Knights serve as a finely tuned defense system. These soldiers and their Serfs serve as the archers, water bucket carriers, catapult artillery, oil pot boilers,, swordsmen - you get the idea… Each have their own jobs to do in peace and war time - and their basic directives are governed by an automatic, (autonomic) system of rules and orders.
Blood vessel-bourne messengers exist as hormones (carrying larger decrees - often from far away glands like the thyroid, ovaries, testicles or adrenal glands) and smaller proteins (providing simpler directives that can be sourced more locally or further away). They coordinate with the telegraphed messages delivered by nerves, and break down into “rest’ (parasympathetic) or “work” (sympathetic) modes, with frequent overlap. Since our focus in this series is about the tears, it is important to discuss the basic elements of a tear and where they come from.
At its core, tears are made of water, salts, proteins and oils. Water is by far, the largest portion of a tear and it comes from several glandular sources and is under a complex neural control. Those telegraph lines are fairly buzzing much of the time and their messages are modified by hormones and proteins. Let’s dive into this next week!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Where do tears come from?
In posts past, I’ve spent a lot of time simplifying what is a rather complex process of how we make tears. This process is a bit like describing how we produce blood - and (less the red and clotting stuff), it is related, in that some blood products (antibodies, proteins, and other immune products) apart from salts and water, are shared. In fact, blood is the primary support for the glands making our tears, so that they can do their job - unsurprisingly, those with major blood problems can also have significant tear problems. In future posts, I’ll attempt to unravel some of the mystery and simplify as best I can about this amazing process. For those who crave the fuller explanation, there is an excellent, more physician-level resource available here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10501785/?fbclid=IwAR3V4f230p6T-Ucji0R3CygMOM03vU5WKxkrXAWrq9d0f-opp0uNnSVyeDI For now, I’ll stick to the Sprinkler System and Firehose analogies with tears being the lifeblood and the blink being the heartbeat. I still like the “salad dressing” and the “salt water” for our describing the two types of tears - but next week we can get a bit more granular with it. Until then, blink strong!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Why rub your eye?
Above video comes from: Defeat Keratoconus @defeatkeratoconus4856 and illustrates what happens to your eye when you rub it - much as you might see with Superman’s (or Superwoman’s) “X-Ray vision.”
Rubbing your eyes can feel good - and generally doesn’t have any immediate negative consequences - so it must be good for us - Right? Well, generally speaking, it’s more wrong than right. Watching the above video gives a unique perspective on what is going on when you do rub your eyes, but let’s consider the good and the bad.
Good news first. When you rub your eye, it is possible to help your eyes make tears. Pressure on the lids can force some oil out of the oil-producing (Meibomian) Glands and oil is an important (and often lacking) part of a tear. I’ve covered much of the benefits of oil in our tears - as well as the function and support of these glands - in many prior posts, so won’t dwell on it here. This pressure can also slightly irritate - and therefore stimulate - the “firehose” glands that create the gush of salty water useful for washing dust, pollen or other irritants out of the eyes. Like a cough, rubbing eyes can trigger the vagus nerve that can slow our heart rate. Mild slowing can help relieve a sense of stress, though major slowing can risk dizziness or even fainting - so this can be a good or bad side effect depending on how slow you go. I tend to separate the act of gentle wiping (generally good for spreading eyelash cleansing products around the lashes, removing loose lashes and excess tears from the lids) from the act of rubbing (exerting force against the eye by firmly pressing on the lids, as in this video - and the subject of this posting).
Bad news can be many - and magnified by underlying eye issues. When you rub your eye, it is possible to damage the cells making and repairing the collagen fibers that create the fabric of the cornea. Collagen is “woven” throughout the clear front part of the eye that we call the cornea, in a distinct pattern that “cross links” these fibers tightly together. With equal woven patterns across the entire tissue, any force inside or outside the eye is “shared” equally across the entire “fabric.” Rubbing can unlink and stretch out these fibers and appears to damage the cells that normally repair this “fabric.” Triggering the defense system from excessive rubbing can also lead to the release of histamine (responsible for itching) that may lead to a vicious cycle of rubbing (similar to scratching an itch that then itches all the more). As we pour our inflammatory chemicals into the tears bathing our eyes, these can ultimately work against good tear production (and aggravate the corneal cells and fibers further). As the fibers become loose in areas most affected, the resulting weakness in the cornea will result in an outward “bowing” of the cornea - called a “cone.” Instead of the perfect spherical, desired “roundness” of the cornea, any bowing will distort the cornea leading to misshapen images (astigmatism) requiring stronger glasses or contact lenses to reshape the images necessary to good vision. At the extreme, this “cone” shape is called “Keratoconus” and can so distort the images that surgery to replace the cornea (a corneal transplant) or special procedures (to restore corneal cross linking) may be required.
More bad news is that too much pressure applied for too long may permanently damage the optic nerve (connecting the eye with the brain). This type of damage is commonly called glaucoma and if unchecked, can ultimately result in irreversible blindness. How much is “too much” will depend on many factors, including genetic tendencies for this nerve damage, or any pre-existing damage (from glaucoma or other injuries to the nerve). Also, if you watch the video carefully, you may see the outward bulging of the sclera (or white part of the eye) behind the cornea. Inside that area exists the thinnest and most delicate part of the retina. In patients with an already thin retina (often referred to as lattice degeneration), stretching the retina - especially in these already thinned areas - may lead to tears or holes that can progress to a retinal detachment - and require delicate surgeries to repair (or result in blindness if unchecked).
Lastly, I’ll point out that putting fingers or other objects in close proximity to the eyeball elevates the risk of transferring germs, toxins, allergy-producing materials or dirt into contact with the eye itself. A common cause for “pink eye” is the spread of germs or other materials from such contact. Obviously any time we touch our lids with our fingers, we are taking such risks unless we’ve carefully washed and otherwise disinfected them first. Ironically, one of the causes of acutely irritated and red eyes in the wake of the pandemic, is the inadvertent transfer of hand sanitizers from freshly “cleaned” fingers that then gets into the eye from alcohol or other germ-killing residue in the sanitizer (ANYTHING GREAT AT KILLING ANY AND ALL GERMS IS ALSO PRETTY GOOD AT KILLING OFF CELLS ON THE SURFACE OF THE EYES, TOO!).
My personal. experience is that I am also guilty of occasionally “rubbing” my eyes - and although I am generally cautious about hand cleaning and not rubbing excessively, I may have caused myself a case of pink eye in the past. When my eyes itch, my preference is to use antihistamine (anti-allergy) eye drops, a clean, cool compress and only mild wiping when applying lid cleaning products (Zocuwipes and Avenova being my favorites), since common lid germs can also aggravate eyes and lead to dryness and irritation. Hot compresses are also useful when dealing with non-itchy, dry or otherwise irritated eyes and when applying the (Bruder or other) heat mask, I use only the pressure required to keep the heat in contact with the lids (and not forcibly press on the eyes). Strong blinking and forced eye closure (short of grimacing) are likewise useful at expressing the Meibomian oil glands (and doesn’t require firm finger-pressure, as in the above eye rubbing video) - so there are ways to relieve an otherwise tired, itchy or irritable eye without resorting to “the rub!”
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
What’s up when the “sprinkler system” dries up?
While I’ve posted about Autoimmune Dry Eye Diseases (an extensive series starts here: https://www.eyethera.com/blog/sjogrens-disease-autoimmune-dry-eye-part-1) and on degrees of Aqueous Tear Deficiency (ATD, starting with a post on inflammation here: https://www.eyethera.com/blog/segment-10-aampb-what-we-know-about-inflammation ) separately before, I’ve been asked recently about determining causes for severely poor tear volume (common to ATD) when the autoimmune tests are not revealing. Knowing that the worst ATD is often associated with Autoimmune Diseases, it is usual to suspect autoimmunity at work, but sometimes all the testing related to autoimmunity comes back “negative” or “borderline” and we are left wondering what else is going on.
I posted on my favorite test for ATD (as part of a series on dry eye testing) here: https://www.eyethera.com/blog/what-do-dry-eye-tests-mean-part-7-tear-volume-and-how-we-measure-it and I’ve included some of my thoughts on causation in all of these prior posts. This week, I’ll attempt to summarize some of this information and offer some renewed insights.
I often use artistic license in my analogies and apologize in advance to those who can appreciate my oversimplification of complex topics. Having said that, I proceed to do the same here. Recalling that the surface of our eyes are covered in living cells that need support to survive, I point out that tears are the “lifeblood” of that surface. Job number one for their survival is that they must be kept moist and we have two means for that. One is what I like to refer to as the “emergency backup system” or “firehose” - the large tear glands that can pour salty water over our eyes (and often down our cheeks). Being salty water, this tear is not much more than moist support - so we have what I call the “sprinkler system” - the number Two means for support - but this group of cells and glands provide the 24/7 “clear blood” defined by a lot of water, with some salts, proteins and oils added in (a kind of clear-blood-like “salad dressing” - where the watery stuff is covered by a layer of oils that doesn’t “mix” with the water - so can act as an evaporative shield).
The emergency backup “firehose” will draw water from our bodies to the last drop, to make that salty solution, but the sprinklers are very sensitive to our overall level of hydration. If we get a little dry, they get dry and the drier we get, the drier they can get. This was first brought home to me when conducting an early study on clogged oil gland (MGD) treatment, where we had to exclude patients with severe ATD. The cutoff was 6mm on the Schirmer’s test strips and a young nurse who was both a friend and known MGD patient came rushing in from dropping off her kids at school to get screened for a treatment under this protocol. Sadly, her Schirmer’s numbers were around 3 and 4mm - well below the 6 we needed to see. On further discussion, she admitted to having had only a cup (or two) of coffee since rising and was obviously “under hydrated.” I advised she return after consuming a couple of quarts of water and we’d try again. Fortunately, re-testing came in around 8 and 9mm and we were able to proceed with the study treatment.
When I find numbers less than 10mm, I dig deeply into water consumption habits - including the “anti-waters” (things that encourage peeing and dehydration) like caffeine, alcohol and the host of medications that can dry us out. When less than 6mm, it is time to also look harder for sources of inflammation. Autoimmunity is the king (or queen) of inflammation, as it can single out water-producing cells and effectively kill them off - resulting in body-wide damages to tissues and organs dependent on their water production (commonly leading to eye, brain, gut, reproductive and joint issues, among others). Dry mouth, with severe, related dental issues, is common to Sjogren’s (perhaps the leading cause of autoimmune dry eye), so asking about a dry mouth can frequently lead to identifying this cause. Since autoimmunity is still relatively poorly understood, it is hard to know the exact portions of populations affected and likely varies widely through the many nature and nurture variables. Ocular Cicatricial Pemphigoid (OCP) appears to be a relatively uncommon cause of autoimmune dry eye, but since it can only be diagnosed through a biopsy of affected conjunctiva (the membrane on the surface of the white part of the eye), it is probably significantly under-diagnosed. Similarly, Sjogren’s is perhaps best identified by a biopsy (of salivary glands inside the lip area), so since most are not subjected to this level of testing, it is hard to know how many patients might be revealed as “positive” this way. Other autoimmune diseases can affect these water glands. Reactions to some medications can trigger an autoimmune dry eye (as well as affecting the moist membranes throughout the GI tract), called Stevens Johnson Syndrome - but since this can occur at different levels of severity, it can also likely be under-diagnosed (the full blown illness is extraordinary in its ability to inflict damages and usually requires hospitalization - but at that level of presentation it is hard to miss). Graft versus host reactions in those who receive tissue transplants fall into a similar spectrum. In the end, the key is what we can do for these autoimmune-diseased patients and while we are coming up with better protocols all the time, we are still sadly lacking in a definitive treatment plan for many.
Dr. Elizabeth James, a PhD in Medicine and Healthcare, gives a good rundown of causes of dry eyes and dry mouth without having an autoimmune disorder or thyroid problems, here: https://qr.ae/pKzfYt I began an answer to treating dry eye-related inflammation here: https://www.eyethera.com/blog/segment-10-b-when-we-are-at-war-with-ourselves but it is clear that we need to determine “root causes” of inflammation in order to best treat it and I advise working with a good dry eye specialist to help (often in concert with a team that should include your Primary Care Provider and may include Rheumatology, Endocrinology, Gastroenterology - among others as the findings require).
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
More for 2024 (2 new dry eye medications in the pipeline)
Alcon ( a pharmacy that “grew up” with eye care-related pharmaceuticals and has evolved into a major player in the world of dry eye treatments) has been testing a new drop for dry eye care, known so far, as AR-15512 (a “transient receptor potential melastatin 8 (TRPM8) agonist,” for those in the know). This group of compounds can stimulate the nerves responsible for the sensation of cold temperature and appears to regulate the production of tears. Early work with menthol showed it could trigger this response - but even small doses applied to the surface of the eye would cause irritation and it was deemed unlikely to be useful - despite its ability to make eyes tear. Subsequent compounds have been tested and found to be less irritating and more useful in provoking tear production. Early Alcon studies of this medication have been named “Comet” and the most recent Comet 2 and Comet 3 studies have continued to be promising - enough that Alcon aims for its application to the FDA by mid-2024. Stay tuned for more on this! (links about this here: https://www.optometrytimes.com/view/positive-results-reported-from-phase-3-comet-trials-of-alcon-s-ar-15512-for-dry-eye?utm_source=sfmc&utm_medium=email&utm_campaign=01132024_OD_eNL_Dave%20Kading%20CBR%20TD_IKA%20house%20ad&eKey=ZWphY2NvbWFAYW9sLmNvbQ== and https://escholarship.org/content/qt2gz2d8s3/qt2gz2d8s3.pdf?t=qaeax8 )
Last week, I gave a nod to Stuart Therapeutics and their phase 3 studies of a polypeptide they call ST-100 or Vezocolmitide. This week, “Okyo Pharma announced positive safety and efficacy data from its phase 2 trial of OK-101 ophthalmic solution, a lipid-conjugated chemerin peptide agonist designed to reduce pain and inflammation in patients with dry eye disease.” Recalling that peptides are the building-blocks of proteins, and that our bodies are made up of countless proteins, it is perhaps no surprise that any substance that can direct protein production or affect protein pathways can likely influence tears (containing proteins) and the surface of our eyes (also regulated by proteins). This new drug was shown in phase 3 studies to improve the signs and symptoms of dry eye disease. Stay tuned for more on this! (links about this here: https://www.healio.com/news/optometry/20240109/ok101-achieves-dry-eye-disease-sign-symptom-endpoints-in-phase-2-trial#:~:text=1%20min%20read-,OK%2D101%20achieves%20dry%20eye%20disease%20sign%2C%20symptom,endpoints%20in%20phase%202%20trial&text=Okyo%20Pharma%20announced%20positive%20safety,patients%20with%20dry%20eye%20disease. and https://www.optometrytimes.com/view/positive-phase-2-results-of-ok-101-for-dry-eye-disease-revealed-by-okyo-pharma?utm_source=sfmc&utm_medium=email&utm_campaign=01132024_OD_eNL_Dave%20Kading%20CBR%20TD_IKA%20house%20ad&eKey=ZWphY2NvbWFAYW9sLmNvbQ== )
Lastly, in response to numerous concerns raised during 2023 about contaminated eye drop products that caused eye infections and even deaths, the FDA has revised its guidelines. Optometry Times provided the following information: “This revised draft guidance revises guidance of the same name from October 2023, “Quality Considerations for Topical Ophthalmic Drug Products.” Specifically, the revision discusses microbiological considerations related to product sterility for all ophthalmic drug products subject to current good manufacturing practice (CGMP) requirements. It is intended for the prevention of contamination of ophthalmic drug products packaged in multidose containers.1
Quality considerations for ophthalmic drugs such as gels, ointments, creams, and liquid formulations such as solutions, suspensions, and emulsions, intended for topical delivery in and around the eye, are addressed in the revision.” Initial interpretation of earlier guidelines caused some manufacturers to believe the FDA rules did not apply to over the counter products and this revision makes it clear that these current good manufacturing processes apply across the board to prescriptive and OTC products. The expectation is that this should help prevent future eye injuries. A link to the FDA guidelines here: https://www.optometrytimes.com/view/fda-challenges-quality-requirements-for-ophthalmic-drugs-with-revised-draft-guidance?utm_source=sfmc&utm_medium=email&utm_campaign=01132024_OD_eNL_Dave%20Kading%20CBR%20TD_IKA%20house%20ad&eKey=ZWphY2NvbWFAYW9sLmNvbQ==
Some helpful eye drop safety information shared by Rebecca Petris of the Dry Eye Foundation: https://www.dryeyefoundation.org/
Lastly, for tips on keeping your eye drops sterile and safe, this video link was also shared: https://www.eyedropsafety.org/news/blog/preservative-free-eye-drops-how-to-reduce-the-risk-of-bacterial-contamination
Stay safe!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463