Blog
More for 2024 (2 new dry eye medications in the pipeline)
Alcon ( a pharmacy that “grew up” with eye care-related pharmaceuticals and has evolved into a major player in the world of dry eye treatments) has been testing a new drop for dry eye care, known so far, as AR-15512 (a “transient receptor potential melastatin 8 (TRPM8) agonist,” for those in the know). This group of compounds can stimulate the nerves responsible for the sensation of cold temperature and appears to regulate the production of tears. Early work with menthol showed it could trigger this response - but even small doses applied to the surface of the eye would cause irritation and it was deemed unlikely to be useful - despite its ability to make eyes tear. Subsequent compounds have been tested and found to be less irritating and more useful in provoking tear production. Early Alcon studies of this medication have been named “Comet” and the most recent Comet 2 and Comet 3 studies have continued to be promising - enough that Alcon aims for its application to the FDA by mid-2024. Stay tuned for more on this! (links about this here: https://www.optometrytimes.com/view/positive-results-reported-from-phase-3-comet-trials-of-alcon-s-ar-15512-for-dry-eye?utm_source=sfmc&utm_medium=email&utm_campaign=01132024_OD_eNL_Dave%20Kading%20CBR%20TD_IKA%20house%20ad&eKey=ZWphY2NvbWFAYW9sLmNvbQ== and https://escholarship.org/content/qt2gz2d8s3/qt2gz2d8s3.pdf?t=qaeax8 )
Last week, I gave a nod to Stuart Therapeutics and their phase 3 studies of a polypeptide they call ST-100 or Vezocolmitide. This week, “Okyo Pharma announced positive safety and efficacy data from its phase 2 trial of OK-101 ophthalmic solution, a lipid-conjugated chemerin peptide agonist designed to reduce pain and inflammation in patients with dry eye disease.” Recalling that peptides are the building-blocks of proteins, and that our bodies are made up of countless proteins, it is perhaps no surprise that any substance that can direct protein production or affect protein pathways can likely influence tears (containing proteins) and the surface of our eyes (also regulated by proteins). This new drug was shown in phase 3 studies to improve the signs and symptoms of dry eye disease. Stay tuned for more on this! (links about this here: https://www.healio.com/news/optometry/20240109/ok101-achieves-dry-eye-disease-sign-symptom-endpoints-in-phase-2-trial#:~:text=1%20min%20read-,OK%2D101%20achieves%20dry%20eye%20disease%20sign%2C%20symptom,endpoints%20in%20phase%202%20trial&text=Okyo%20Pharma%20announced%20positive%20safety,patients%20with%20dry%20eye%20disease. and https://www.optometrytimes.com/view/positive-phase-2-results-of-ok-101-for-dry-eye-disease-revealed-by-okyo-pharma?utm_source=sfmc&utm_medium=email&utm_campaign=01132024_OD_eNL_Dave%20Kading%20CBR%20TD_IKA%20house%20ad&eKey=ZWphY2NvbWFAYW9sLmNvbQ== )
Lastly, in response to numerous concerns raised during 2023 about contaminated eye drop products that caused eye infections and even deaths, the FDA has revised its guidelines. Optometry Times provided the following information: “This revised draft guidance revises guidance of the same name from October 2023, “Quality Considerations for Topical Ophthalmic Drug Products.” Specifically, the revision discusses microbiological considerations related to product sterility for all ophthalmic drug products subject to current good manufacturing practice (CGMP) requirements. It is intended for the prevention of contamination of ophthalmic drug products packaged in multidose containers.1
Quality considerations for ophthalmic drugs such as gels, ointments, creams, and liquid formulations such as solutions, suspensions, and emulsions, intended for topical delivery in and around the eye, are addressed in the revision.” Initial interpretation of earlier guidelines caused some manufacturers to believe the FDA rules did not apply to over the counter products and this revision makes it clear that these current good manufacturing processes apply across the board to prescriptive and OTC products. The expectation is that this should help prevent future eye injuries. A link to the FDA guidelines here: https://www.optometrytimes.com/view/fda-challenges-quality-requirements-for-ophthalmic-drugs-with-revised-draft-guidance?utm_source=sfmc&utm_medium=email&utm_campaign=01132024_OD_eNL_Dave%20Kading%20CBR%20TD_IKA%20house%20ad&eKey=ZWphY2NvbWFAYW9sLmNvbQ==
Some helpful eye drop safety information shared by Rebecca Petris of the Dry Eye Foundation: https://www.dryeyefoundation.org/
Lastly, for tips on keeping your eye drops sterile and safe, this video link was also shared: https://www.eyedropsafety.org/news/blog/preservative-free-eye-drops-how-to-reduce-the-risk-of-bacterial-contamination
Stay safe!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
What’s new in 2024? Let’s focus on the nerves!
Dompé corneal nerve graphic for Oxervate
Another pipeline first!
Stuart Therapeutics has started a study for dry eye treatment using a novel approach. As you recall from my earlier posting - tears are made of water, salts, proteins and oils (I use the salad dressing analogy here – but it is perhaps more correct to see tears are a form of “clear blood” to nourish, support and protect the surface of the eyes). Most current treatments aim to reduce inflammation by interfering with inflammatory pathways (steroids, cyclosporine, lifitigrast and the like). This supports tear production, but has its most profound effects on tear volume (reducing the damaging effects of inflammation on the water-producing cells). Most include moisturizers and some include oils (Castor oil for Restasis, or the novel, solely artificial oil in Miebo). Cyclosporine also has been found to promote protein production from the mucin-making goblet cells. Salt production is well regulated but becomes unbalanced through evaporative loss of water and resulting toxically-high salt concentration, so adding moisture in artificial tears is a standard strategy.
Stuart Therapeutics new product is a “polypeptide.” Polypeptides are made from strings of amino acids called peptides – which are the building blocks of proteins found throughout nature. Diverse as a group, they are known to help with the many functions required for a healthy life. This new, synthetic group of amino acids they call “PolyCol,” appears to assist in building up or repairing damaged cells within the ocular surface. This includes the nerves beneath the epithelial surface as well as helping restore surface cells. Corneal nerves are the “maestro” that helps coordinate the “symphonic” production of tears from the “orchestra” of cells and glands that make those tears. These nerves are also responsible for the constant upkeep or repair of corneal surface cells – so it is no surprise that other approaches to dry eye includes the repair of those damaged nerves (see my post on related neurostimulation https://www.eyethera.com/blog/what-is-neurostimulation-for-dry-eye-treatment-and-do-i-need-it ).
Dompé is a company marketing a recombinant form of human nerve growth factor (NGF) they call Oxervate, which has been a staple of eyedrop therapy for patients with damaged nerves leading to a condition called “Neurotrophic Keratitis” (or NK). When the maestro is lacking, the tear quality and volume suffer, as do the surface cells maintained by those tears. Chronic “open sores” (ulcers) can form, and corneas deteriorate. Since the nerves are “broken” there can be chronic pain from the remaining swollen “stumps” of those nerves – or the corneas can become “numb” as feeling is lost. Sadly, the higher pain centers can become so overburdened that a chronic pain can exist independent of the state of the surface nerves and cells. See my link to this topic here: https://www.eyethera.com/blog/why-do-my-eyes-hurt-even-though-my-eye-doctor-says-they-look-fine
Current treatments that align with this new product include Autologous Serum Tears, Platelet Rich Plasma drops, Oxervate (as noted above), amnion products and any other forms of “Neuro-Stimulation” as I noted in the earlier post (including Tyrvaya nasal spray and iTear). Adding a new angle that doesn’t require blood draws and frozen storage, or hyper-expensive and often hard-to-dispense drops (Oxervate, with its syringe to meter the drops), blurry “contact lenses” made of human-derived membranes (amnion) or frequent sneezing (Tyrvaya) will be most welcome! It is also true that it sometimes requires a number of these products to turn around these difficult problems - so adding another “arrow to our quiver” of useful therapies is always good news! For a full physician-level discussion of the new product, see this link:
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Why do my eyes feel tired all the time?
From: https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/computer-vision-syndrome?sso=y
First - Happy New Year! I hope 2024 is the year for great advances in dry eye care - and I want to be a part of that evolution! My contribution on these pages will continue to be my blogging efforts to educate and raise awareness - and in my dry eye specialty practice - my commitment is to continue to offer leading edge technologies and treatments. Today let’s focus on “tired eyes.”
“Tired eyes” is a common complaint among dry eye sufferers. There are several likely reasons for this and I can enumerate a few of them here. I’ll start by reposting an answer I made to a patient with “a little conjunctivochalasis” (CCH) who asked if this could cause tired eyes:
Yes - partly because of the relationship to dry eyes (which increases blink rates - a bit like running a marathon all day), partly due to the poor distribution of the poor tears (causing increased dry eye symptoms - that drain you and also cause eyes to want to close). Dealing successfully with the dry eye problems can sometimes offset the CCH-related fatigue enough, but sometimes it is still necessary to fix the CCH. I have a lot of posts on CCH on my eyethera.com/blog
Blinking is central to eye health and can occur at rates from 2-50 times per minute - as observed in human studies (Monster AW, Chan HC, O'Connor D. Long-term trends in human eye blink rate. Biotelem Patient Monit. 1978;5(4):206-22. PMID: 754827.) Remember that a key motivator to spontaneous, involuntary blinks are the “dry spots” forming on the surface of the eye - and - at a subliminal level - causing irritation to corneal nerves that become exposed by the evaporation of the tear film overlying those nerves (leading to the dry spots). Dried out cells become injured (or dead) and allow them to “stain” with some of the dyes I referenced in my dry eye testing series of blog posts. (See: https://www.eyethera.com/blog/more-on-staining-the-surface-of-a-dry-eye-and-what-it-means) When there is a problem with tear oils (too little or too poor a quality - including those oils tainted with soapy residue from germ byproducts), then the oil’s “liquid Saran Wrap” benefits are lost and the water leaves (evaporation). This means that a lack of good oil will lead to a rapid blink rate (trying to keep up with that evaporation). This in turn, is that “running a marathon” effect that can tire out the blink-muscles and make eyes “feel tired.”
The fine muscle movements required to keep eyes focused and coordinated for the myriad activities we require them to do, make eye muscles the most active muscles in our entire bodies. “Considering that we make at least 100,000 saccades alone each day, it is not surprising that many extraocular muscles are very resistant to fatigue.” (Wong, Agnes M F, 'Eye Rotations, the Extraocular Muscles, and Strabismus Terminology', Eye Movement Disorders (New York, 2008; online edn, Oxford Academic, 12 Nov. 2020), https://doi.org/10.1093/oso/9780195324266.003.0007, accessed 1 Jan. 2024.) Saccades are the back and forth eye swings - that among other things, are the swift movements we use to read text like this. We also have pursuit movements, where we cause our eyes to follow objects around (like tracking traffic while driving). Add to this the blinking and emotive muscle movements of the eyelids and you have an Ironman/Ironwoman-level of activity going on daily for most of us. An interesting treatise on blinking and exercise can be found here: more about blinking (Paśko W, Zadarko E, Krzeszowski T, Przednowek K. Relationship between Eye Blink Frequency and Incremental Exercise among Young Healthy Men. Int J Environ Res Public Health. 2022 Apr 5;19(7):4362. doi: 10.3390/ijerph19074362. PMID: 35410042; PMCID: PMC8998332.)
Another consideration is that when eyes become irritated (as from dryness), their most protective reflex is to close. As eyes dry out, they become progressively irritated and this produces a stronger urge to close (and rest) them. Forced prolonged use of eyes (as is frequent in this digital era) encourages more closures to reduce this level of strain and the closing of eyes is part of sleeping. Fatigue is a strong incentive to sleep and we can equate eye fatigue and this need to close them, as a “tired feeling.” Physical fatigue refers to the muscles getting tired. Mental fatigue has to do with reducing the ability to concentrate. When eyes become constantly irritated from dryness, this constant, annoying “buzz” at higher levels in the brain appears capable of inducing a degree of mental fatigue (and another reason for eyes -and their owners - to “feel tired.”) Following the 20/20/20 rule (see the excellent article by the American Optometric Association: https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/computer-vision-syndrome?sso=y) , getting sufficient sleep and taking care to make the best of tears will help ensure your eyes feel less tired at the end of these increasingly longer days, now that we’ve passed through the 2023 Winter Solstice. Here’s to a great 2024!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Happy Holidays and Getting To Know Dr. J
First - Happy Holidays! For people suffering with dry eyes (or any chronic disease), it can sometimes be hard to have your best celebration for any occasion, but many professionals (including me) are working hard to deal better with this (otherwise if untreated) chronic, progressive disease.
Getting to know Dr. J is a video co-produced by (my wife and I’s eldest grandchild) Ladybird Slater for a school project for her college, the University of New Hampshire. I don’t get the chance to discuss dry eye (most will sigh with relief over that), but it does give a glimpse into my past and present life. Hope you like it (we think she did a great job!)!
Getting to know Dr. J
More about CCH (When the eye’s white surface turns to a washboard and tears have an obstacle course…)
I was recently asked how important the fornix is to Conjunctivochalasis (CCH) and should it be restored in CCH surgery.
The “fornix” is the reservoir or “well” that contains our best tears, in that those tears have yet to be used for supporting the exposed surface of the eye. The exposed tear is becoming the old, used-up, dried up, dirty tear that needs to be replaced and a blink is that “heartbeat” that renews that support by turning over that tear. So preserving the fornix is important. (We want a deep well, capable of holding a lot of healthy, fresh tears.)
Some technologies that excessively burn and damage the conjunctival tissue that has come loose and otherwise “rides up” (shortening the fornix) can risk “over-tightening” and foreshortening the reservoir (shortening the depth of the “well.”) Higher levels of heat, applied in broad swaths, can cut, burn and scar down that membrane. In my experience, radio frequency can straddle the line between tightening and over tightening - and can seal the conjunctiva over the white of the eye (sclera) without damaging the reservoir function. The lighter degrees of heat can be applied in serial, linear passes - sequentially shrinking and “shrink wrapping” that membrane - with just enough of a “burn” in places as to heal and “stick” the membrane back in place.
Excess burning causes higher levels of scarring and tightening, which may, for some patients, risk significantly reducing that fornix. An alternative is cutting away the excess conjunctiva and either allowing it to then heal - or gluing amnion over the exposed white tissue (sclera). Either can restore the fornix but doesn’t fix the problem (MGD and evaporative dry eye) causing the problem (CCH).
Off-label use of RF as described in my studies, has been shown to improve MG function, so combining both the RF plication (shrink wrapping the membrane) with the RF -heated expression of wax-clogged glands has made more sense to me. There are some relative contraindications to RF (an active cardiac pacemaker being one), so there are times where I’ll turn to alternative methods.
Some of my posts relating to CCH, including this most recent post here:
https://www.eyethera.com/blog/can-conjunctivochalasis-get-better-without-surgery
And my earlier series on CCH - part 3: When do we treat CCH – and what are the non-surgical options?
Jun 12
Written By Dr. Edward Jaccoma, MD
https://www.eyethera.com/blog/cch-part-3-when-do-we-treat-cch-and-what-are-the-options
Conjunctival Chalasis (CCH) part 2 - How do we fix it?
Jun 5
Written By Dr. Edward Jaccoma, MD
https://www.eyethera.com/blog/conjunctival-chalasis-cch-part-2-how-do-we-fix-it
What is Conjunctival Chalasis (CCH) and why should I care?
May 29
Written By Dr. Edward Jaccoma, MD
https://www.eyethera.com/blog/what-is-conjunctival-chalasis-cch-and-why-should-i-care
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Eyedrops and Glaucoma - a new study supports clinical observations
Antihypertensive Eyedrops Trigger Dry Eye Disease, Corneal Damage
September 19, 2023
https://www.ophthalmologyadvisor.com/topics/cornea-ocular-surface/antihypertensive-eyedrops-trigger-dry-eye-disease-corneal-damage/
This study supports the common clinical findings many dry eye doctors see in their clinics on a daily basis - and which have been demonstrated and validated by earlier studies. THE LAST THING I WANT TO DO IS BASH THE USE OF DROPS TO CONTROL GLAUCOMA. I’ve published on this before https://www.eyethera.com/blog/jwk8lv0558b5ewcp7cxummr7pusblv and https://www.eyethera.com/blog/dry-eye-cataract-and-glaucoma-segment
I think it is important when studies like this are published, to point out that glaucoma is a potentially blinding disease and that dry eye is much less likely to result in blindness. Job number one is to prevent blindness and I routinely prescribe drops to treat glaucoma. Fortunately, SLT (laser) and Durysta implants are often a good way to avoid glaucoma medication and when we have to turn to drops, increasing numbers of “preservative free” drops are now available to reduce the negative impact of these drops. Various operations exist to also reduce dependence on drops (It was interesting to read in this same study, that substituting surgery for drops did not significantly reduce the dry eye impact - but this might be predicted knowing that surgery promotes inflammation as part of the healing process and requires frequent use of topical steroids, antibiotics and other medications that fight inflammation at the expense of adding preservatives and other chemicals to the surface of that operated eye).
I find that many glaucoma patients received relief from the burden added by glaucoma drops, by increasing the amount and quality of their tears, using the protocols I’ve commonly used for that purpose. It makes sense to me that patients with robust surface health - largely thanks to having excellent tears - will tolerate their glaucoma drops better than those who have poor quality tears and an already disrupted, damaged ocular surface. I would urge any patients who require daily topical medication (like glaucoma patients on glaucoma drops) to get a good dry eye evaluation and institute any recommended treatment at the same time they begin their eyedrop treatments.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Why do my eyes hurt - even though my eye doctor says they look fine?
This is a fairly common question I hear in my dry eye center, and the answer can be complex. No one answer fits all eyes or all eye pain, but the usual name given to this group of complaints is “pain without stain,” implying the eye looks normal, so there is no obvious cause to the pain described by the patient.
A few weeks ago I posted about “pain without stain” here: https://www.eyethera.com/blog/testing-part-8-miscellaneous-testing-the-good-the-bad-and-the-ugly-side-of-testing As I mentioned, this opens the door to a portion of dry eye patients with complex problems that are often overlooked or passed over, as our ability to effectively detect, diagnose, and treat this problem remain limited. Treating pain is an important part of a doctor’s duty and dry eye doctors are constantly looking for better tools to fill this toolbox.
One increasingly off-label utilized medication is Naltrexone – in the news as an emergency rescue drug for those who overdose on opioids like Fentanyl. Due to the complex nature of how our bodies deal with pain, we have our own versions of opioids - and the receptors for these innate chemicals exist in nerves and tissues occurring throughout our body.
In numerous prior posts, I’ve covered the role of irritation from dryness activating our natural defense (immune) system, leading to inflammation and initiating the “viscous cycle of dry eye disease.” Corneal nerves become damaged and abnormal – which can lead to chronic pain. Treating the dry eye can reduce irritation, but in some cases the damage to the nerves appears to be too great and the pain lingers. Low Dose Naltrexone (LDN) has been shown to reduce inflammation and has been helpful in curbing pain in a number of chronic, painful conditions such as fibromyalgia and MS. Recent research has shown that LDN eye drops appeared to improve tear production in rats who were made diabetic, with related diabetic dry eye disease, so there may be a number of benefits to the way this drug can reduce inflammation. Zagon IS, Klocek MS, Sassani JW, McLaughlin PJ. Dry eye reversal and corneal sensation restoration with topical naltrexone in diabetes mellitus. Arch Ophthalmol. 2009 Nov;127(11):1468-73. doi: 10.1001/archophthalmol.2009.270. PMID: 19901212; PMCID: PMC2840396.
In a recent post from Glance By Eyes On Eyecare https://glance.eyesoneyecare.com/ a new product for neuropathic corneal pain was announced as under investigation. The following is an excerpt from a physician-level communication I received from them:
“Are there any new treatments for neuropathic pain?
OKYO Pharma Limited announced it has submitted an investigational new drug (IND) application for the development of OK-101 to treat neuropathic corneal pain (NCP).
What is OK-101?
OK-101 is a lipid-conjugated chemerin peptide antagonist of the ChemR23 G-protein coupled receptor, which is typically found on immune cells of the eye and is responsible for the inflammatory response.
How does it work?
OK-101 was developed using a membrane-anchored-peptide (MAP) technology and has been shown to produce anti-inflammatory and pain-reducing activities in mouse models of DED and NCP.
Didn’t OKYO already file an IND for OK-101?
Good memory! And yes—back in November 2022. However, this IND was for DED, not NCP.
As for updates on that application… in April 2023, the company activated the first U.S. clinical trial site for its first-in-human (FIH) phase 2 multi-center, placebo-controlled trial of OK-101 for DED, which was followed by randomized dosing of participants in June 2023.
How about for NCP?
According to the company, preclinical data from a ciliary nerve ligation model on mice found that OK-101 reduced NCP response similar to that of gabapentin (a common oral drug used for such pain), administered via intraperitoneal injection.
The model supported the topical administration of OK-101 as a potential non-opioid analgesic for NCP.
Gotcha. So what’s next?
Pending FDA acceptance, the company—in partnership with Boston-based Tufts Medical Center—is planning to launch an open-label phase 2 study in Q1 2024, with an anticipated 40 patients to be enrolled.
And the significance of this?
With no current FDA-approved drug on the market to treat NCP, this second indication for OK-101 could become the first, proving to be a game changer for patients suffering from this chronic condition.”
I should add that I don’t have any “insider knowledge” about OK-101, but I’d guess that it comes out of the research-information obtained from studying the natural opioids in humans (also known as endorphins, enkephalins and dynorphin-related “natural painkillers”). I welcome any additional tools to this important toolbox as current approaches remain all to limited!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Even Dry Eye Specialists get the Blues.
As a mentor to other dry eye doctors, I am sometimes asked why certain treatments “fail” to improve their patients. Even dry eye specialists can get confused (and depressed) when their best efforts fail to help their patients, and since this question is relevant to that issue, I thought I’d post one of my recent answers.
The question I answered went something like this (paraphrased): “I’ve used frozen, preserved amnion contact lenses (Prokera) to treat a good number of patients with SPK, only to find they continue to have SPK – what am I doing wrong?” The doctor went on to detail some of the dry eye treatments used for these patients, including night ointments and nighttime patching, lots of artificial tears, cyclosporine or lifitegrast, Tyrvaya (the nasal spray that stimulates tear production), lotemax (a topical steroid) for flares and home therapies or Low Level Light Therapy (LLLT) to manage the Meibomian Gland Dysfunction (MGD).
One treatment I discussed in an earlier blog referred to using Amnion membranes to help heal damaged eye surfaces (see here: https://www.eyethera.com/blog/what-to-do-when-the-surface-of-your-eye-gets-broken-scratched-operated-on-infected-or-otherwise-damaged ) - which applies to the Prokera referenced in the question above. Amnion is the tissue surrounding a baby growing in a mother’s womb, and the influence it has on the baby is both nourishing and generally supportive of helping the baby grow quickly and healthfully in that womb. As such, I’ve referred to using these membranes as a means of “putting the eye back in the womb” to help heal surface damage.
https://biotissue.com/products/ocular/prokera/#prokera-form Image of the popular “Prokera Slim.”
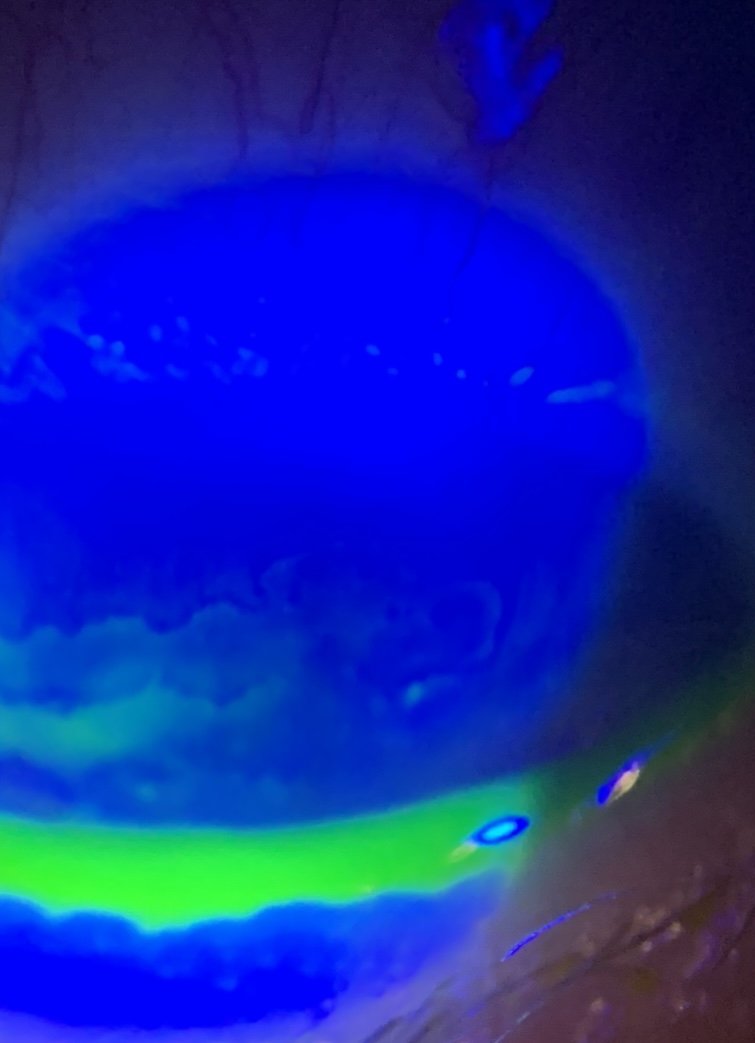
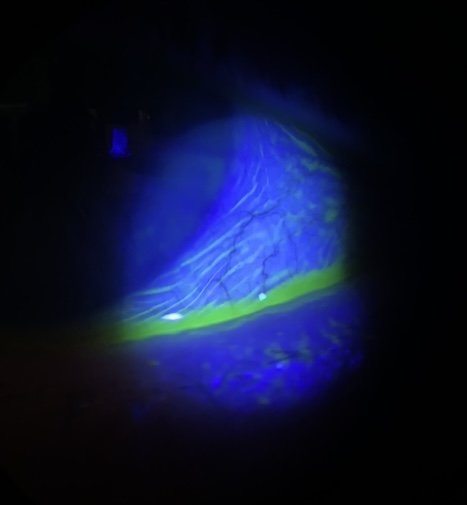
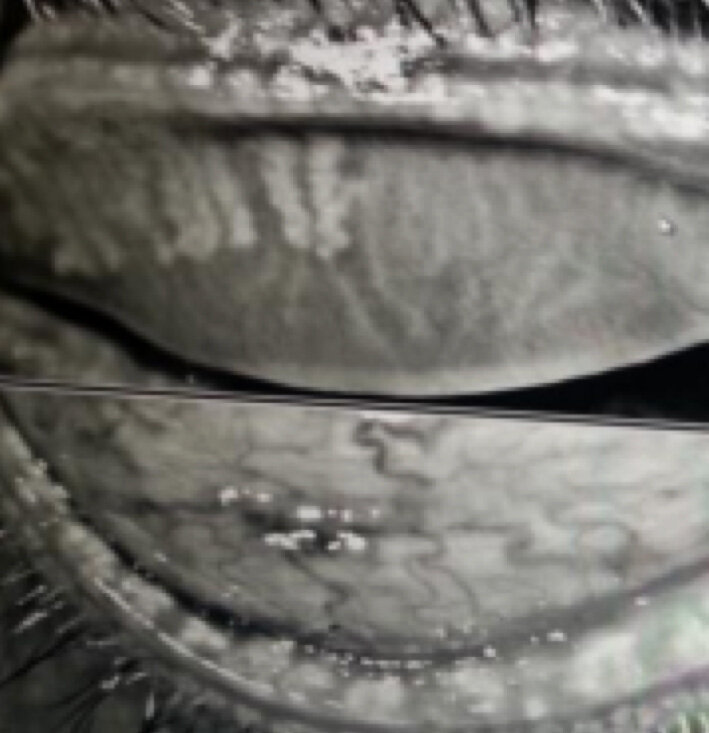
Superficial Punctate Keratopathy, or “SPK” is the common finding in many types of eye-surface diseases (and refers to groups of damaged cells on the surface of the eye which are best seen using a microscope and fluorescein dye - see photo)
The photo was taken through the eyepiece of an examination microscope using an iPhone camera after applying a drop of fluorescein dye and using a blue filter. This patient has a geographic area of “torrid SPK” on the illuminated cornea, that looks a bit like a leaning chess rook, with some patchy, more typical SPK to the right of that “rook.” Looking further, we can see a small “divot” or “notch” in the margin of the lower eyelid, which is a common finding following the healing from a stye (this patient had a long history of them). We also see a little “foam” in the pit of that notch (indicating bacterial activity leading to inflammation of the lid and eye). Harder to appreciate in this blue-light image are blood vessels crossing the margin of the lower lid (squiggly lines) and dilated blood vessels on the white of the eye – all indicating degrees of inflammation – in this case a combination of evaporative dry eye disease, rosacea and related blepharitis (irritated eyelids).
- but the main cause remains dry eye disease, which is a many-faceted beast. Anti-inflammatory medications including Cyclosporin (Restasis, Cequa, etc), Lifitigrast (Xiidra) and steroids (like Loteprednol) are used to treat dry eyes because they are good at reducing Aqueous Tear Deficiency (ATD = too little water being produced) but are not great at improving evaporative dry eye from Meibomian Gland Dysfunction (MGD). In my practice and in large clinical studies, MGD is the leading cause of dry eye, though it can couple with ATD. Prokera is great for giving a jump start on healing a dry eye-damaged surface, but unless you deal with all the ancillary, co-contributing issues, the SPK is likely to be only partially improved or to recur quickly. LLLT can help some MGD, but as most MGD is obstructive and most obstructions involve waxy plugs, unless you are clearing these plugs (and a substantially heated expression appears the best way to do it), then you're not going to get very far.
Apart from waxy plugs (common in early stages of MGD), there are scarring issues (well described by Dr. Steven Maskin) that can begin as "periductal fibrosis." This can require probing to make good headway. Rosacea is a common cause of the non-obstructive versions of MGD and here, IPL (Intense Pulsed Light – see my earliest posts on this here: https://www.eyethera.com/blog/not-so-secret-weapon-of-dry-eye-treatment-intense-pulsed-light-or-ipl ) can really shine (and LLLT may play a positive role). Getting appropriate degrees of buy-in from patients, in doing required levels of "homework," is always key to anything else (including Prokeras) you can offer. You mentioned home therapies - I include oral Omegas 3-6-9 capsules, Heat masks and lid crunches (unless the primary issue is Rosacea), and lid hygiene products (HOCL and a cleanser like Zocuwipes or Cliradex products).
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Revisiting Thyroid Eye Disease (another look at TED)
TED is not this patient’s real name but the acronym as described below. The rights to this photo belong to the company making the treatments described below and in this link: Tepezza
I see a number of patients with Thyroid Eye Disease (TED) as the bulging of the eyes causes high degrees of exposure and related dry eye disease issues. While traditional and advanced dry eye treatments can help with that aspect of this troubling disease, a recent treatment option emerged, called Tepezza. In an physician-spec ad (annotated by me in parenthesis) from a group called MDNB (mdnbupdate@mdnbupdate.com), about this drug:
“TEPEZZA® (teprotumumab‑trbw) has demonstrated proven efficacy for the treatment of TED in clinical studies.1‑3 To help gauge results, the Clinical Activity Score (CAS) is used as a diagnostic tool to identify the signs and symptoms of inflammation characteristic of TED. CAS is a 7‑point composite score, measuring spontaneous orbital pain (unprovoked pain behind and around the eye socket), gaze‑evoked orbital pain (pain caused by otherwise normal eye movements), eyelid swelling, eyelid erythema (redness), conjunctival redness, chemosis (swollen membranes over the white of the eyeball), and inflammation of caruncle or plica (swelling of the membranes at the inner corner of the eye). A lower score indicates fewer symptoms.4
The CAS is a composite score with equal weighting of a number of factors and may be required for treatment approval. However, the factors may not be of equal clinical weight to patients or to physicians treating those patients.
Select Important Safety Information:
TEPEZZA may cause infusion reactions. Infusion reactions have been reported in approximately 4% of patients treated with TEPEZZA. Reported infusion reactions have usually been mild or moderate in severity. Signs and symptoms may include transient increases in blood pressure, feeling hot, tachycardia, dyspnea, headache, and muscular pain.
Patient 2 before treatment
Pretreatment2
Proptosis (the degree of bulging eyes): 24 mm
Diplopia (double vision): 0
CAS: 5
Eyelid swelling
Eyelid erythema
Inflammation of caruncle/plica
Conjunctival redness
Chemosis
After treatment
Posttreatment (Week 24)2
Proptosis: 19 mm
Diplopia: 0
CAS: 1
Eyelid swelling
Patient 5 Before treatment
Pretreatment 5
Proptosis: 25 mm
Diplopia (double vision): 3
CAS: 5
Spontaneous orbital (eye socket) pain
Gaze-evoked (looking around) orbital pain
Conjunctival redness
Eyelid swelling
Eyelid erythema (redness)
After treatment
Posttreatment (Week 24) 5
Proptosis: 21 mm
Diplopia: 0
CAS: 0
No inflammatory signs and symptoms
Individual results may vary.
Both patients were treated with TEPEZZA in a clinical trial.
Both patients completed a full course (8 infusions) of treatment with TEPEZZA.
Both results shown are with no surgical intervention.
Help get your patient started on TEPEZZA
TEPEZZA is the first and only FDA‑approved treatment for Thyroid Eye Disease (TED)1,6, regardless of TED activity or duration. Review these steps for starting your appropriate patients on TEPEZZA here.”
_______________________________________________________________________________________
These results are compelling (while marketing will always showcase their best before and afters, I believe the majority of treated patients experience real results), so this sounds like really good news, and I think it is - as I mentioned in my earlier post on this topic here: https://www.eyethera.com/blog/8lemgnwt0bqqd15fmqr9ljrkdfe420. However, in various meetings I had with experts in San Francisco at the American Academy of Ophthalmology event 2 weeks ago, it appears that the effects are prone to “wearing off” - in as little as a year and a half. Retreatment can be done, and so far, appears to still be effective. Since it is such a novel and new medication, we are still learning about it – including (as I mentioned in my earlier post) its ability to cause permanent hearing loss in some individuals. Fortunately, this side effect appears relatively rare and monitoring hearing may give early clues that can lead to discontinuation before hearing is fully lost or steer us away from using this particular treatment in patients who already suffer from severe hearing loss.
One of the bigger problems is the cost, as a single course of typically 8 infusions can run into the hundreds of thousands of dollars (I heard as much as $340,000 from one expert and costs can vary greatly from region to region). This is mostly borne by insurance companies and is partly due to the cost of how it is given – requiring specialized staff to administer intravenous infusions (usually at “infusion centers”). The company is investigating allowing patients to give the medication below the skin in small injections - like a diabetic giving themselves insulin, as this method appears to be safe and effective in limited trials. Ultimately these costs filter down to everyone covered under these insurance policies, which can drive up costs for all – so I’m glad there may be a cost-effective alternative. Of interest was statements made by these experts that the age-old treatments, including oral steroids and radiation therapy, can offer similar benefits that appear to be more durable, so if Tepezza isn’t available to some, or eventually proves ineffective for many, then the older treatments are still likely to be of benefit. More encouraging was that a number of other “biologic” medications are being investigated for treating TED - which means more options may soon be available (and hopefully this will drive costs down and increase access).
From current clinical experience, many will be spared expensive, painful and potentially risky surgeries to decompress eyes by removing bone and the soft tissues swollen behind the eyes - by this new medication – so having a medical treatment that also avoids steroid and radiation side effects is still a very welcome addition to our medical treatment options!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
Testing Part 8 – Miscellaneous testing: the good, the bad and the ugly side of testing
The previous 7 parts of my testing series identifies some common testing strategies we employ – but is hardly comprehensive and really can’t be, since this field evolves almost daily.
It would be a stretch for every dry eye specialist to have every tool in the dry eye toolbox and the time to do every test, not to mention the cost, would be all-consuming. I’ll touch on some peripheral testing strategies and then speak to some of the common shortcomings we can run into. Good testing is when the tests lead us to a better understanding and then better treatment of a disease. Bad testing is when the tests can mislead us - and Ugly is what we get when we are lead down misleading, unnecessary “rabbit holes” - wasting time, resources and potentially harming our patients.
Patients who have “Pain without staining” are a special group – largely because pain is considered a subjective issue – but also because staining (with the stains mentioned in the earlier part of this series) can vary with something as simple as the weather (drier weather promoting more evaporation and dryness). But pain is a tough metric, mostly because doctors are still grasping at understanding the full gamut of pain – from the initiation of the sensation, up to the brain’s reception and interpretation of that signal. Unlocking this puzzle is getting a bit better understood and can start with a simple test - first of creating some degree of an uncomfortable event (touching the cornea with something that should register a degree of sensation – the cotton wisp, the fishing line, or some chemical such as increasingly stronger solutions of salty drops, or the common numbing drops that feel stingy before they numb).
Once we determine that there is the ability to sense some degree of “pain” at the surface, then we typically numb the eye with drops and see if the sensation of pain goes completely away. If it does, then this suggests something at the surface level and confocal microscopes are leading the way in showing swollen, inflamed nerves even when the surface “looks OK.” If the pain does not go completely away, then this implies a higher-level disorder – pointing to how certain pain centers in the brain can become amplified to where they can apparently “reverberate” or continue to signal pain (kind of like the thumb that throbs even when it appears to have recovered from a whack - you feel it, but you can’t see something wrong with it – at least unless and until it swells and turns hot and red). Sometimes all it takes to resolve this kind of pain is the therapy to make more and better tears - and to give it time to settle down – but sometimes time doesn’t heal it and it still hurts. This will be the focus of a future post as it is a complex and significant problem.
When the Schirmer’s is very low and we suspect Sjogren’s Disease (see my earlier posts on autoimmune disease, starting here: https://www.eyethera.com/blog/sjogrens-disease-autoimmune-dry-eye-part-1 ), the testing is imperfect at best. Hearing that the mouth (along with nose, throat, the GI tract and in women, the vagina) is extremely dry, along with the very low Schirmer’s, will often trigger a blood test and possibly a lip biopsy – but if everything is “negative” (and we’ve effectively ruled out other causes like certain medications and the common “anti-waters,” like too much caffeine and alcohol), then we may put a diagnosis like “clinical Sjogren’s” on it. Typically, I’ll treat it like Sjogren’s and have referred some to rheumatologists in case we missed something. Sometimes what was “negative” on lab testing may eventually turn “positive,” so this remains a bit of a “dark science.” Fortunately, there continues to be a lot of work in the medical field to help us find a better way to diagnose and treat these “autoimmune dry eye diseases.”
Because many metabolic, nutritional, and hormonal disorders can cause a constellation of health-related issues that include dry eye disease, it is often necessary to involve a larger group of specialists to sort this all out. Running wider batteries of lab testing can sometimes provide the necessary diagnostic clues to sort this out – and sometimes a good history can save a lot of lab testing – so history is key. Once we identify the prospect of associated diseases or metabolic imbalances, it is common to refer patients to the appropriate specialists in that field. Working as a team typically can afford patients the best outcome. As doctors continue to subspecialize in ever narrowing aspects of disease, we rely on them to teach less specialized doctors what they need to know to best serve their patients. These related subspecialties may include OB-GYN, Endocrine, Rheumatology, GI, ENT, Neurology, Dermatology and Allergy to name a few.
I can briefly touch on a couple of other common problems with testing and how I currently approach them:
- First, is the issue with Meibomography – covered in the first segment of this series on testing. It appears the InfraRed (IR) cameras commonly used to image Meibomian Glands are best able to show the “active” portions of the glands. This can make it hard to see portions of the glands that may still be present and otherwise healthy enough to “recover” their function. Patients and doctors can get overly nervous when presented with the pictures that show nearly (or wholly) absent gland tissue – yet on so-called “transillumination” the doctor may uncover substantial evidence of residual, less apparent gland presence. At least one Meibomography unit utilizes the combination of both direct-IR and transillumination technologies (Lipiview). Fortunately, a dark room, a slit-lamp (an eye doctor’s typical microscope) and a small flashlight can do a similar exam when paired with the IR photography – so a better idea of the likely level of recovery is available to most dry eye centers. Another issue with meibography is the inability to sort out the source of obstructions. Many times it is the common “waxy plugging” that may be visible at the level of the doctor’s microscope. Other times it may be from scaring or keratin plugs. (check out my earlier post on this here: https://www.eyethera.com/blog/why-do-expensive-dry-eye-treatments-fail-and-what-is-maskin-probing ) These are critical pieces of information, and technology-driven companies continue to innovate in this field – so more and better devices are continually coming into the dry eye specialist’s equipment marketplace.
- Second is the issue with drug interactions, medicamentosa and tachyphylaxis (a lot of confusing words!). Drug interactions seem self-explanatory, suggesting when two or more drugs react together, the sum of their effects (good or bad) can be amplified – or negated. The nature of their effects can turn in a fully new direction from the expected effect of either alone. As the field of medicine expands and the number of drugs continue to grow, this issue can (and does) quickly get out of hand. Computers and databases can (and do) help, and most pharmacies offer advice when their computers pick up the possibility of such interactions – but not all interactions can be known as some are uniquely dependent on a patient’s genetics and other disease states. Lastly, a drug interaction does not have to require another drug to “interact with” – as they can simply interact with the patient’s underlying genetic makeup or allergies to cause their unwanted effects. Using the history of which medications a patient is currently on as well as past history (especially anti-oil-gland medications like Accutane or some intentionally toxic medications like anti-cancer drugs), is necessary, since even relatively short courses of some medications can leave a long-term, dry eye imprint in their wake.
Medicamentosa is basically an unwanted reaction to a product, or the vehicle used to apply or carry the product. This product can be a single drug, cosmetic, preservative or even an “artificial tear,” where it causes an ill effect. It can also be an ill effect caused by a combination of drugs, cosmetics, preservatives or the oxidation caused by the interaction of air with the product (in or out of a bottle). This problem appears to be more common that I think most of us realize. One such example can be seen in glaucoma medications, where a single, or in some cases, multitude of drops - applied to reduce eye pressure, can “gang up” on the surface of the eye, causing redness and irritation. These drops can be necessary to prolong the quantity of vision but can reduce the quality of vision and therefore of life. Sometimes the problem is with the preservatives and sometimes it is the drug itself - or a combination, that causes this grief. It is up to the prescribing doctor to help sort this out and to hopefully find alternative ways that can be less toxic to the eye.
Tachyphylaxis is when the eye becomes “used to” a medication so that it requires more and more of that medicine to achieve a similar effect. Drops that cause blood vessels to squeeze (to reduce redness) are an example of this problem. As the drops wear off, the “rebound” of redness requires more frequent applications to get a similar effect (until even continuous applications may not be enough to reduce redness). See my earlier posting on this problem here: https://www.eyethera.com/blog/can-i-use-eye-whiteners-like-visine-or-lumify-when-my-eyes-get-red
The best way to resolve medicamentosa or tachyphylaxis issues varies, but we often have to require our patients to stop all medications, drops and products (never do this without the blessing of the prescribing doctors involved in your care) and then take a fresh inventory of the patient’s problems before adding them back. This is usually done by adding them back one at a time, to discover which are the more offending. Sometimes there are well known issues with medications and/or patterns of reactions that are immediately obvious to the dry eye specialist who can then more easily identify the likely culprit – so best to seek out a good one who can help in this regard.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
What do dry eye tests mean? (Part 7) Tear Volume (and how we measure it).
Probably the simplest test I do every day is – for me – one of the most important tests I consider in every dry eye evaluation. It has been around for over a century and involves a numbing drop and a tiny piece of filter paper placed along the edge of the eyelid for 5 minutes. It is called the Schirmer’s test and the reason I find it so useful is because it gives a reasonably accurate idea of the output of the “sprinkler system.” This helps to rapidly breakdown the source of dry eyes from one of two common pathways (that often intersect).
Simplistically, we can look at dry eye from the standpoint of tear quantity and tear quality. It can become very complicated when we look at what that means – but as dry eye doctors, we assess “Aqueous Tear Deficiency” or ATD and “Meibomian Gland Dysfunction” or MGD. ATD means not enough water and MGD means not enough (or not good enough) oil. This is important as treatments for one, generally are very different from the other. Since many patients have a degree of both, for simplicity’s sake, we might focus on the one that is the greater when the patient wants a stepwise approach (I like to advise tackling both simultaneously when clinically indicated and the patient is willing).
I have explained much of this in my earlier posts, and I always recommend that beginners go to the beginning of these posts to get updated. For regulars – or those in a hurry – I’ll point out that the “sprinklers” make the “good tears,” rich in water, salt, proteins, and oil (the “salad dressing”). The “emergency backup system” or “fire hose,” makes the salty tear water that floods the eye if it gets too dry, otherwise irritated, infected, damaged or if we emotionally cry. Numbing the eye helps to “turn off” this firehose reflex and allows the “sprinklers” a chance to do their job for the 5 quiet minutes we soak up that “salad dressing” tear.
Since most of this “good tear” (the “salad dressing” or “clear blood-like product”) is made of water, we can consider this the “Aqueous Tear” and too little leads to ATD. Fixing this nearly always involves drinking more water (to be fully hydrated). The obvious flip side is to also avoid too much “anti-water” (anything that encourages excess peeing – like caffeine, alcohol and many medications like antihistamines for allergies and sleep aides, decongestants for sinus congestion and cold pills, “water pills” for swelling and high blood pressure (check with your doctor prescribing these medicines to see if there are alternatives that would be safe for your health issues) – and the list goes on and on (bladder control pills, some mental health pills, high blood sugars as in less controlled diabetes, etc. etc.). After achieving a good water balance, the next step is reducing inflammation, as inflammation is particularly hard on the water producing cells involved with the Aqueous Tear production.
The number I like to see on this test is 15 millimeters or more – though patients under 30 years of age will often make 30mm or more, and the normal production levels tend to fall as we age. PRETTY MUCH EVERYONE SHOULD MAKE 10MMs OR MORE. This is because it takes about this much just to reasonably cover the surface of the eye (though more “open” eyes may need more - and less open eyes may get by with less). This helps understand how patients with excessively open eyes (like in Thyroid Eye Disease, or after “too good” a lid lift operation) can suffer even with “normal” tear amounts, as well as explaining why patients with droopy lids may tolerate relatively poor tear volume (and why a treatment for severely dry eyes can be the lateral tarsorrhaphy, where we surgically, partially close an eye for reducing exposure as added protection of the cornea). Punctal plugs may sometimes become indicated in this group (see my earlier posts on damming up the tears).
A common pitfall of this test is that it does require a careful attention to details to get a valid “number.” This involves making the surface sufficiently “numb,” (often harder to do when the surface has become overly sensitive from chronic dry eye damage and may require multiple drops), to turn off the “firehose” tear system. Then it is key to appropriately “dry” the gutter in the lower lid, to remove excess moisture (from the numbing drops and any patient-produced tears, so we can start from ground zero to measure only freshly made “sprinkler system” tears). Turning the room lights down also helps avoid glare-related reflex tearing and is better done early in this process. I start the “stopwatch” the moment I’ve finished drying this “gutter” (usually with a sterile QTip rolled gently along the floor of that “gutter”) and I’ve prepared the strips for placement at the start of the preparation for the test – so they are ready to go. A “Pro Tip” I learned, is to fold the outside edge of the strip for the right eye, so once placed and subsequently removed, it is easy to see which eye produced what result. Placement of the strips is along the outer (ear-side) edge of the lids so that the cornea is not directly impacted by these drying papers (avoiding extra stimulation of the firehose, as well as avoiding even minor damage to the cells on the cornea).
When the number is 6mm or less, it is sometimes not possible to effectively turn off the fire hose, as that has become the primary tear when the sprinklers are unable to produce enough tears. This is because the surface of the eye must stay moist to survive – when cells get dry, they die and drop off, exposing the underlying nerves and causing the pain these patients experience routinely. This is another “Achilles Heel” of the test – since we may get high numbers when we expect lower ones – but this can be inferred from other markers (like surface staining, tear salt levels and the microscopic evaluation of the tear layer along the lower lid if there is not too much conjunctivochalasis or CCH – as the “gasket effect” of that membrane can block the gutter-like reservoir in the lower lid from holding the normal volume of better tears and keeps the tear layer artificially high). It is also true that we will usually get similar numbers between the two eyes (unless one eye has had a unique problem, such as a single-eyed infection, injury, or surgery) – so if the two eyes have a similar history, we can usually expect a similar result on the test. When one is “abnormally high” when the other is “abnormally low” then it generally implies the higher one is artificially elevated by reflex tearing, and we go more by the lower one.
When the number is 10 or more (and we think this is a true reading), then we focus on the oil issues. Those patients should still stay well hydrated, since water levels can be quick to vary - and adding low volume to an otherwise poor tear oil is a recipe for ocular surface disasters. Making more and better oil generally requires eating good oil, doing good blinks, keeping that oil free flowing and keeping germs at bay, that would otherwise eat those oils and pollute those tears with byproducts of their digestion (What I call basic dry eye “Homework.”) Too much “germ poop” in the tears will lead to a vigorous immune response that can damage the tear glands and drive more ATD and MGD.
I’ve posted many times on our best tools for improving oils beyond this simple “Homework” – and this generally includes unclogging the oil (Meibomian) glands – with a heated expression - when the clogging is the typical, waxy plugs acquired early in this MGD disease (called evaporative dry eye). When they have been clogged for “too long” (which appears to vary by patient), there is a tendency to either develop “styes” (chalazia, as in an “acne pimple-like” cyst) or (more commonly) for the glands to silently wither and develop deeper levels of scarring that can “cut off” the glands. Scarring, if partial and mild, appears to respond to Intense Pulsed Light (IPL) and gentle, heated expressions. If the scars are more severe, then they often require probing (small, piano-wire-like tools used to “roto-rooter” the glands open). IPL also appears uniquely suited for stimulating the glands, reducing inflammation (by killing germs, mites and closing dilated blood vessels pouring the body’s “napalm, hand grenades and bazookas” into the tears, as a response to the irritation and damage caused by germ poop and dryness) and warming the glands to help in thinning the oils (though it doesn’t seem to keep the oil hot enough, long enough, to allow optimal expression – so I often advocate for following IPL treatments immediately, with an effective form of heated expressions).
Science is always looking for better tests - and a benchmark, century-old test is ripe for replacement by a “newer tool.” There is a test measuring “Lactoferrin levels” in tears, utilizing a tiny sample of tears, like the salt-level test. Lactoferrin is a common protein found uniquely in these “sprinkler system tears.” Low levels are more common in dry eyes and very low levels may indicate a higher risk of autoimmune dry eye (Sjogren’s being the usual one). It has been compared favorably to the Schirmer’s test and is now commercially available. Being relatively new, it remains to be seen how this will fit into the usual dry eye evaluation and cost remains an issue (the cost of a tiny piece of paper and a numbing drop is negligible and this newer test is not). I’ll keep you posted on this test as I develop some familiarity with it!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
What do dry eye tests mean? (Part 6) Inflammation (and how we measure it).
Inflammation is at the heart of dry eye disease. This is relatively obvious, as dryness causes irritation and irritation begets inflammation - fueling the vicious cycle of dryness and damage.
Red Right eye inflamed from glaucoma medications and dry eye disease - left eye had Durysta implant to reduce glaucoma medications - redness and dryness improved!
At the surface of the eye, inflammation causes redness, heat, swelling, pain and ultimately loss of function. The redness is a product of dilated blood vessels and the heat is a byproduct of increased blood flow. Dilated vessels carrying “defense products” from our immune system, will cause the vessels to get leaky - and the oozing of fluid through these leaky vessels causes swelling. The defense products (I like to refer to as “human napalm, handgrenades and bazookas” - but are really called cytokines, chemokines, antibodies and ultimately white blood cells) will put pressure on -and cause irritation to - the nerves around them (causing pain). This stimulates reflex tearing and leads to blurring vision - and may ultimately inflict damage to the eye’s surface. This warfare will affect the cells and glands that would make the “good tears” leading to increasing levels of salty tears and dryness - eventually damaging the cornea (or clear window of the eye - so loss of function). And this all relates to “common dry eye” - whereas autoimmune dry eye takes this to an entirely higher level (by adding ““human smart bombs” to the off-kilter immune defenses, aimed at the water producing glands - see my posts on this here: https://www.eyethera.com/blog/sjogrens-disease-autoimmune-dry-eye-part-1 through part 5 here: https://www.eyethera.com/blog/ogh4ia5gewpejt9cszlk0emeccuzh3
The “Need to know” has pushed science and technology to develop tests and time-tested methods to help detect and measure degrees of disease - and dry eye disease is no stranger to this need. The simplest method to detect inflammation is observation - looking for redness, heat, swelling, and surface damage. Pain is more subjective but the sense of irritation and pain is best tracked with validated questionnaires (see my first post on testing here: https://www.eyethera.com/blog/what-do-dry-eye-tests-mean ). Surface damage is commonly measured with staining dyes and excess salt levels quantitated in testing I’ve discussed in this same series. Some Keratographers (Oculus R-scan) allow more objective measurements of redness and thermal imaging cameras can provide information on heat elevations from inflammation.
Inflammadry Test kit (positive test indicated by pink stripe with blue control)
One of the newer tests for inflammation involves a rapid, in-office test that looks for a certain immune system “biomarker” that has been shown to be common to the dry eye pathway of inflammation, so-called “matrix metalloproteinase 9” (MMP-9). Quidel makes this test - called “Inflammadry” - and using a technique familiar to most, it looks like a “CoVid test” in terms of a blue control mark and a pink positive mark. Like the CoVid test, itis either positive (pink) or not (no pink) - so it is not a quantitative test (there is no gradient validated to measure the amount of MMP-9 in the tear - only that it meets or exceeds a certain amount considered abnormal). There is a Dacron spongy segment that needs to sit against the conjunctival membrane of the eye and “soak up” enough of a tear sample to give an accurate reading. The initial study report states: “As MMP-9 is a nonspecific marker, many conditions other than DE (Dry Eye) can produce a positive result. This information is found in the package insert and includes conditions such as recent ocular surgery, infection, or allergic conjunctivitis. The package insert further states that false negative results can occur in the setting of systemic immunomodulators, topical or oral steroids, cyclosporine, tetracycline, and topical azithromycin, all of which may inhibit metalloprotease activity. The test should be avoided in patients with cicatricial conditions that could lead to conjunctival injury or allergies to cornstarch, Dacron, topical anesthetic, or fluorescein dye.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5580996/
Because the majority of my dry eye patients have obvious amounts of inflammation and have eyes that are already uncomfortable from dryness, I’ve generally found this test to be more uncomfortable for the patient than the worth of reading a “positive” test (and if it’s negative, I’m not sure I always believe that, since many are already on some type of anti-inflammatory treatment and some are so dry it is hard to collect enough tear for a valid sample). Once a method becomes available to get a quick read on the amount of MMP-9 (hence the degree of inflammation present), then I’d be more inclined to want to measure that (especially if it was as easy and less irritating, as the salt testing I mentioned in the last post). Of interest to me, one of the more common pathways for MMP-9 to become elevated is for the salt levels to rise and “stress out” the cellular surface of the eye - so when the salt test shows high levels of salt, then a positive MMP-9 test can also be predicted.
More helpful, can be the Quidel test for the adenovirus common to causing pink eye (viral conjunctivitis). Since an eye can turn “pink” for a large number of reasons (including dry eyes and/or to many preserved drops like artificial tears or glaucoma medications - like my patient above) - and since this virus is extremely contagious, it can be useful to identify a viral cause when it exists (treating redness with a steroid makes sense when the redness is from dry eye-related causes, but using a steroid to treat a viral cause can allow the virus more time to evade the healthy immune response and cause the eye greater grief when the steroid is withdrawn). This test is also like a CoVid test (and a nasal swab for CoVid is often also indicated, since that virus is another highly contagious cause for pink eyes these days).
One of the reasons eyes can feel relatively “normal” even when many of our dry eye tests appear to show even severe levels of dry eye disease, has to do with corneal sensitivity. I touched on this point in my earlier blog post here: https://www.eyethera.com/blog/the-hill-of-sorrow-and-how-getting-better-can-sometimes-feel-like-getting-worse It is especially helpful to evaluate for reduced sensation of the eye’s (corneal) surface when we see this “disconnect” between how a patient reports they feel and how we think the eye probably should feel. A variety of tests are evolving to help detect and then quantitate this feeling - from as simple as asking if a patient feels a typically irritating drop when it is placed on the eye (and grading that response on a scale of 0-10), to testing with wisps of cotton, fragments of fishing line or pulses of air. Confocal microscopy (a special microscope that can scan the cornea with high magnification) can help detect abnormalities in the nerves that can help further explain such relative “numbness.” Fortunately we now have many tools to help bring nerves back (as nerves are important to the production of tears and serve as a necessary impulse to good blinking) - and the “Hill of Sorrow” post helps explain more about that, too!
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
What do dry eye tests mean? (Part 5) Salt & why you don’t drink seawater.
As I noted in the prior testing segments, the Tear Break Up TIme (TBUT) is an indication of evaporation - and gets shorter (less time until evaporation) when the oil doesn’t “seal in” the water. The flip side of evaporation, is that only the water leaves - which means the stuff that is otherwise dissolved in that water remains behind. Since tears are salty by nature (and the fire hose is mostly salt water), the salt levels can climb quickly under conditions favorable to evaporation of tears. The ultimate conditions favoring evaporation are dry, windy air. Add to that, conditions that favor having eyes more open and you have a recipe for toxic levels of salt in the tears.
Salt levels are measured in terms of. “osmolarity” - a chemical term that quantifies the amount of salt in a solution. The higher the number, the more salt in that solution. Every cell in your body is subject to salt levels and blood carries a “normal” salt level of 275-295 “milliosmoles” of osmolarity. This is a reflection of the desired salt levels inside every cell in your body - and the surface cells on eyes are no different. Once salt levels rise above the level of salt inside the cells, water will seep across the cell’s border membranes in the direction of the salt, to “normalize” the salt on both sides of that membrane. As a result, cells “dehydrate” - becoming crinkled, shriveled up ghosts of themselves - before giving up the ghost completely. (Sorry, it is getting close to Halloween and ghosts must be on my mind).
Most know that if you get stranded at sea, the last thing you should do is drink the seawater, as it will only dry you out further and make you progressively more thirsty (until you get sick and die from thirst). Salt levels in tears can concentrate to levels higher than seawater and risk drying out the surface to toxic levels. Our “firehose” tears will become necessary to wash all that salt away - but those tears are not the “complete” tears from our “sprinklers” (which make water, salt, protein and oil) - so our surface gets progressively weaker, more damaged and drier.
Many dry eye specialists will measure salt levels with a tiny “bird-beak-like” device that dips into the tears lining your lower eyelid and “sips” a tiny amount of tears into the tip. A commercial unit found in many offices is the “TearLab” and their website offers additional information for those who wish to dive deeper (see the link below). Their device has a “test card” calibrated with a range of electrical elements that measure the flow of electricity across that salty water (higher salt levels conduct faster and better than lower) and gives a precise level of salt in the tears measured in those milliosmoles (mOsm/kg). Normal levels in tears range from 280-295, but once it climbs to 308 or more, it starts to become “toxic.” 316 -324 is “bad” but we commonly see levels higher than the salt-testing machine can register (it goes up to almost 400 and then becomes too high to measure). I find those with the highest levels to generally have the worst oil and faster evaporation (a TBUT generally less than 3 seconds and often less than 2 seconds).
Since TBUT is a good proxy for evaporation-related dryness (which is a proxy for poor oil), you might wonder why we would bother to also check tear salt-mOsm. Some patients have very active “fire hoses” which can largely keep up with salty elevations. Since each eye is separated on sides of the face and can have differing degrees of evaporation related to “which way the wind blows,” as well as having variable degrees of oils expressed with degrees of blinking, it is common to see wide swings in salt levels. When both eyes are very high, this can mean trouble with the fire hose keeping up and spell worse troubles for the surface trying to stay healthy. Even a difference of 8 mOm or more is considered significant, since salt is normally so carefully regulated by our eyes (and the consequences can be so great once salt levels get out of whack). High salt levels wreak havoc with the surface, causing burning, stinging, (reflex) tearing, blurring and scratchy sensations - basically every dry eye symptom since high salt leads to drier eyes. Some symptoms from other diseases can overlap with dry eye, so having more lab and clinical findings to help sort out the true causes can be a help.
Many patients ask if they can reduce their tear salt levels by avoiding salt in their diet. While this makes intuitive sense, it isn’t clinically true - again because of the innate, careful regulation of salt levels as part of our normal tear “recipe.” Just like blood is highly regulated, so too are our tears - and for the same reason - cells are delicate and salt levels are important. So the answer isn’t to reduce salt intake (at least for this purpose - check with your PCP if your blood pressure or other health issues might require you to alter the salt in your diet since a certain amount of salt is essential to your health). The better approach is usually to pay more attention to your oil intake and the function of the Meibomian Glands, that make the precious oils for your tears.
For a link to TearLab, see: https://www.tearlab.com/
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
More on staining the surface of a dry eye and what it means…What do dry eye tests mean? (Part 4)
Last week I introduced the orange dye called Fluorescein and how it can color the tears in a way that allows dry eye specialists to monitor the “Tear Break Up Time” (TBUT). I mentioned it also stains dry, damaged cells on the surface of the cornea, so a dry eye doctor can assess the damage being done to the ocular surface by this dry and/or dysfunctional tear. This dye is a vital part of most eye exams and the amount, the timing from when applied to when examined and the dilution (and in what product - from anesthetics to salt water) can all have a bearing on how it stains and how it is perceived. There are patterns of uptake that are characteristic of certain eye diseases - so a skilled dry eye doctor has a lot to consider when interpreting how a dye like this reacts with their patient’s eyes. A blue light filter will help the orange dye “fluoresce” where the staining or puddling orange dye will now look bright yellow, to further highlight irregular and damaged areas on the surface of the eye.
Because a cell has to be significantly damaged in order for the dye to be absorbed into the cell (or to stain the footprint of where the cell used to live - but now is gone), the presence of any “staining” can be significant to the exam. Another common stain used to examine a dry eye is Lissamine Green and it is also non-toxic and generally well tolerated by the dry eye patient. It will stain more mildly damaged cells and is taken up by the conjunctiva more than the cornea (where Fluorescein is taken up more by the cornea and less by the conjunctiva), so is often used in conjunction with the orange dye when assessing damage from dry eye disease (which can affect the entire ocular surface). It doesn’t mix as well with anesthetics, but both can be easily diluted with salt water - and can be delivered in an unpreserved cocktail that should not damage any eye - but can give a better overall image of dry eye (amid other causes of) damage.
Where most areas of the body contain discrete focal points of immune fluid drainage and processing centers called lymph nodes, the eye strains and processes immune fluids through the conjunctiva first. Patterns of swelling in that otherwise clear, thin membrane can indicate various likely diseases which are differentiated into two main groups. Papillae are discrete round “bumps” with a small blood vessel at its core and are typically related to allergies and/or bacterial damage where Follicles are discrete round “bumps” of immune cells that push blood vessels away from the center. Fluorescein dye will “pool” around these bumps, highlighting them in a way that makes them more easily identifiable for the doctor to see. The conjunctiva on the underside of the eyelids tends to react more in this way and it is partly for this reason that a dry eye specialist (or any eye doctor) will often “flip over” eyelids (including the larger, upper lids) after applying some dye.
Friction in the area under the upper eyelid margin will cause a “callous-like” reaction (somewhat akin to the guitar-strummer’s thumb strumming the strings). The green dye will help light this up and it is further evidence of a dry eye (and especially of poor oil, since good oil would help lubricate that margin). Since the leading edge of the lid functions like a “windshield wiper” that helps distribute and replenish tears over the eye, the eye doctor term for this callous is “Lid Wiper Epitheliopathy” (or LWE for those in the know - and for more - see below). Friction over the white of the eyeball can lead to “Conjunctivochalasis” (or CCH) and the green dye can also light up zones around the pleats, folds and wrinkles of that now loose membrane while the orange-yellow dye can puddle along these folds (each uniquely highlighting that issue for the doctor to see). Dryness will damage the more exposed membranes and corneal surfaces first, so a pattern of yellow stippled staining over the cornea with the orange/yellow dye and green stippled staining over the conjunctiva will be more prominent in the average dry eye patient’s eyes.
Fluorescein showing “reverse staining” over clear, raised areas of the cornea known as “Map Dot Fingerprint Dystrophy” (lower left side of image where dye pools around and under the irregular patches that don’t stain in this particular patient - see my link on this topic here: https://www.eyethera.com/blog/5b9vbda1r8e8r5y07l9bslgttcl4d8 as well as a few tiny dry spots (small bright yellow dots). The puddle of yellow-green is the tears lying along the lower eyelid margin that shows the typical irregularities or “notching” common to MGD.
My prior posts on CCH include some of the photos that show how the dye highlights the wrinkles of the otherwise invisible membrane like this one. For a quick link to more on this topic, click here: https://www.eyethera.com/blog/can-conjunctivochalasis-get-better-without-surgery
and here:
This illustration and to learn more at a doctor’s level about lid wiper, see this link: https://www.reviewofoptometry.com/article/lid-wiper-epitheliopathy-what-the-od-needs-to-know
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
What do dry eye tests mean? (Part 3)
In most offices (including the offices of dry eye specialists), it is common to place a drop of orange (fluorescein) dye into each eye, in order to “see” the tears (now stained by the dye) and to see any “dry spots” (where dryness-damaged cells will take up the dye and show the degree of damage being done to the surface of the eye from a lack of good tears). Watching the dye become scattered by drying (evaporation) has been a standard method of judging the quality of a tear for generations (using the doctor’s slit lamp - or examining microscope) and is called a Tear Break Up Time (TBUT). The act of placing a drop of dye in the eye - with whatever “carrier” (some use anesthetic drops while other prefer saline) will “change” the results, because the drop alters the characteristics of the patient’s tear.
Many modern keratographers (instruments used in dry eye centers to investigate the causes of dry eyes) allow a so-called non-invasive tear break up time (NITBUT) measurement. This records the time it takes to see dry spots on the surface of the eye caused by evaporation and is not altered by drops, as it looks with projected light rings on the patient’s eye - to see “breaks” in the rings caused by evaporation (and runs a timer to see how long that takes from the time of a blink). This is considered a more “objective” test (not influenced by the attention span of the observing doctor) and is extremely useful in determining degrees of Meibomian Gland Dysfunction, because MGD means having less healthy oil floating on the surface of the tear. This oil will normally stabilize the tear by preventing evaporation (water has a hard time evaporating through an adequate amount of oil, akin to Saran Wrap sealing moisture from leaving a sealed container in the fridge). Without oil providing the “liquid Saran Wrap” function, comes rapid evaporation and dry spots. These dry spots function like little open sores on the surface of the eye, and are largely responsible for many of the classic dry eye symptoms - as salty tears will irritate these open sores, causing stinging, burning and reflex tearing.
Healthy tears commonly take 20 seconds or longer to begin evaporating (under standard humidity conditions). The “average” inter-blink-interval (the time between blinks) varies with the task and environment. The key driver of the blink reflex is when the cornea has a dry spot. When we are visually engaged (as in staring at computer screens), the brain can “override” the sense of a dry spot and allow considerably longer intervals between blinks (which can result in many dry spots that can interfere with vision and ultimately cause inflammation - as a response to irritation). Under in-office conditions, a “normal” blink interval can be closer to 10 seconds - so in my office we look for a NITBUT of 10 seconds or greater (meaning it should take 10 seconds or longer to see a single dry spot on a staring cornea) to indicate a good tear.
Courtesy of Topcon’s Brochure for their Topcon CA 800 Keratographer (used by the Excellent Vision Dry Eye and Rejuvenation Centers in Portsmouth, NH and Stoneham, MA). The red zones are the driest and fastest to dry - in as little as 3.4 seconds in the Left eye and 5.5 seconds in the Right eye for this “test patient.” Their “Interblink Interval” is 5.2 seconds - so potentially “keeping up” with the Right eye but not the Left’s rate of evaporation. These measurements indicate this patient does not have good tears - and is likely to have significant MGD as a cause of their dry eyes.
As I’ve stated before, a blink is the “heartbeat” of the eye’s surface. https://www.eyethera.com/blog/avoiding-a-heart-attack-on-the-surface-of-your-eye The interval between blinks is critical to maintaining a healthy surface, as frequent blinking can refresh that surface and prevent dry spots - as long as the interval between blinks keeps up with the evaporation and as long as the blinks are sufficiently strong and complete - to engage the oil glands and to fully turn over a tear. Some keratographers can assess that interval, as well as the time to acquire the dry spots - and can provide a graphic analysis that is easy to understand and to track over time.
Unfortunately, many factors can confound adequate measurement of the tear break up time, such as the humidity in the room (less humidity means tears will evaporate more easily into that dry air, vs more humid air), the force of the blink and ability of the blink to express oil from the glands, eye rubbing, recent artificial tears, air currents (fans or air conditioning) that provide fresh dry air to the eyes, and even the amount of germ activity along the lids with enzymes that turn oils into soaps. Even a lot of oil - if contaminated with these soapy residues - can quickly break down and allow rapid evaporation even when the oil otherwise seems fairly abundant. Lastly, some equipment is not up to the task of identifying very rapid blinks, and may continue to run the clock as the computer continues looking for evaporation. A rapid blink can keep the surface from otherwise evaporating, and therefore show a longer Tear Break Up Time (TBUT), than would be clinically true. Fortunately, the older technique of using the orange dye called fluorescein to stain the tears, and then to observe with a microscope during an eye exam can still be useful in identifying the more accurate tear break up time when the computer’s information appears suspect. Additionally, the foam is clearly evident during that exam.
A dry eye specialist will commonly look at computer driven data in the context of their own exam and the history from the patient, to best assess the condition of the Meibomian Glands and the amount and quality of oil they are producing.
To schedule an appointment with Dr. Jaccoma, call Excellent Vision at either of these two dry eye offices:
(1) 155 Griffin Rd, Portsmouth, NH 03801 (603) 574-2020
(2) 3 Woodland Rd, STE 112 Stoneham, MA 02180 (near Boston) (781) 321-6463
What do dry eye tests mean? (Part 2)
One of the reasons to seek out a dry eye specialist, is that to be a dry eye specialist, they should have invested time and money into obtaining and understanding up-to-date, specialty-specific technologies for diagnosing and treating dry eye disease. Thanks to the many engineers, companies and doctors leading the way – there are now MANY such technologies available and virtually no specialist will have (nor are likely to need) all of them.
If you wonder why many specialists charge what seem to be exorbitant prices for their services, it is worth noting that many of the diagnostic technologies cost upwards of $30,000 each and treatment devices can run $100,000 each - and the average clinic will have several such technologies. There are also the usual overhead costs of running such facilities and since inflation has gone up dramatically, hiring and keeping good staff who can run and service these machines, is at an all-time high. There is also a much-needed serious commitment on the part of the doctors (and their staff) to keep up with all of this technology, so in the end, it is never truer said, than: “you are likely to get what you pay for” in this field.
Now with that behind us, let’s get into the more specific dry eye exam.
In my center, perhaps the most useful device we use to examine and educate our patients with, is the so-called keratographer. This multi-functional machine allows us to image the Meibomian (oil) Glands in the eyelids, to monitor their function by determining the “Non-Invasive Tear Break-Up Time” (NITBUT), the “Inter-Blink Interval” (IBI), and to image the surface of the eye with diagnostic dyes (looking for dry spots, and the smoothness – or lack of smoothness – of that surface). It also can read the curvature of the cornea (useful in determining the power of focus of that part of the eye), to measure the volume of tear supported on the lower eyelid and to video the characteristics of the lids during the blink reflex. Some have software to create automated reports that can be used to relay information to the referring doctor or other specialists and may serve as a useful tool for the patient to keep track of their findings.
Imaging the oil glands is critical, as 85% of dry eye patients have a measure of Meibomian Gland Dysfunction (MGD) as a cause. The majority of these have visible abnormalities of these glands when photographed with InfraRed (IR) cameras such as those in the average keratographer. It is common to estimate the percentage of remaining gland tissue from these photos, though I find that IR photography tends to underestimate the amount of remaining tissue, as it appears to highlight only the active, oil-bearing portions (where a technique called transillumination can sometimes reveal what appears to be substantially more tissue). As these glands clog up, they tend to “constipate,” which causes them to dilate (presumably from increasing pressure trying to force their oils around the obstruction), and then to whither (atrophy). The eventual end-result is a loss of the glands and it can be difficult (if not impossible) to fully rejuvenate them with present technologies.
Meibomian Glands appear white, should run the full length of the rolled-over eyelid, and number 25-30 per lid. Most of these MGs are short, withered remnants - indicating an advanced degree of Meibomian Gland Dysfunction (MGD).
This photographic evidence is often alarming – both to the specialists and to their patients – and raises a significant “call to action.” It is hard to refute this level of evidence, even when symptoms and other clinical findings do not seem to appear quite as bad as this would otherwise suggest. What we’ve learned is that even as few as 6-functional glands per lid can provide sufficient oil so as provide a decent tear function. Because we are born with 25-30 glands per lid, this means we can lose up to 20-25 of them before we become aware we have a problem. Now that we are living longer lives, and using our eyes far more than previous generations would (given electricity to light our environments has only been common in households since the early 1900’s and power digital devices we use in all walks of life these days are common only in the last 30 years), it is incumbent on eye doctors to do everything in their power to ensure their patients have tear glands capable of lasting their patient’s lifetimes (and matching their lifestyle demands). I would have a hard time trusting a dry eye “specialist” to provide optimal care without the ability to image these glands. Next week, I’ll discuss some of the other functions of the keratographer and how we interpret these results!
What do dry eye tests mean?
Dry Eye is a complicated disease and testing can be complex and confusing. While I can’t interpret your specific tests, I can give a general idea of what tests mean. It is up to the dry eye specialist performing the tests to give the most accurate interpretation for each specific case.
That said, I will review some of the common tests you might find in a dry eye exam from a dry eye specialist. This list is not fully inclusive of all the tests a doctor might perform nor can I indicate every possible result.
History is perhaps the single most important diagnostic “test” we eye doctors (and really, virtually every doctor) have. Aside from determining the prior history, including any attempts to correct the dry eye problems, a validated questionnaire is very useful as it allows us to get a “number” relating to the degree of dry eye symptoms. While there are many such questionnaires, SPEED and OSDI are perhaps among the most common. Using “SPEED” (from https://eyewiki.aao.org/Dry_Eye_Syndrome_Questionnaires), Standard Patient Evaluation of Eye Dryness Questionnaire (SPEED)
“The SPEED questionnaire was designed by Korb and Blackie in order to quickly track the progression of dry eye symptoms over time.[9] This questionnaire gives a score from 0 to 28 that is the result of 8 items that assess frequency and severity of symptoms. The symptoms assessed include dryness, grittiness, scratchiness, irritation, burning, watering, soreness, and eye fatigue. The questionnaire further assesses whether these symptoms were not problematic, tolerable, uncomfortable, bothersome, or intolerable.[10] The questionnaire also monitored diurnal and symptoms changes over 3 months.[11] Validity of the questionnaire was determined by seeing how well it was able to segregate patients based on their symptoms, relative to the OSDI questionnaire (gold standard). The resulting sensitivity and specificity were 0.90 and 0.80 respectively.[11]”
A score of under 6 is considered minor but may still be associated with significant dry eye disease. The higher the number, the more symptomatic the individual. Because symptoms are so subjective, it is impossible to compare one patient’s symptoms to another. However, because the questionnaire is “validated.” It is likely that changes in a patients self-reported symptoms on this score will accurately reflect changes in their disease. We like to see progressive lowering of this score (indicating likely improvement).
Visual Acuity – probably one of the simplest and most underrated of dry eye tests. While 20/20 is considered “normal,” many eyes are capable of “better” - often as good as 20/15 (indicating what the average person can see at 15 feet, this eye can see at 20 feet). When eyes get dry, the surface gets irregular, and vision will suffer. When blinking affects vision (vision fluctuates with blinking), this is a common sign of dry eye disease. Checking for a glasses prescription is often an exercise in futility, as the variable surface gives variable results with almost every blink. A “Pinhole” is often employed to determine the best correctable vision, as this allows the patient to move the tiny hole over a more regular part of the eye, so vision can be optimal. If glasses are of a recent prescription and the pinhole still improves the vision further, this could be a sign of dry eye (or that the first prescription was incorrect). Other disease states (such as diabetes) can also result in fluctuating vision and an inaccurate prescription, so it is up to the doctor to determine the exact cause of blurry vision.
Another test common to most eye exams is most often included with dry eye exams – measuring IOP (IntraOcular Pressure). While a variety of technologies exist to do this, it is important to measure with the same technology each time as the results commonly vary between technologies but are validated within the same device. Average IOP is approximately 10-20 (or 22, depending on the group and the technology being used), measured in millimeters of mercury by convention. The reason this is important is that many times dry eye specialists rely on steroids to get inflammation under control – but steroids can lead to increased IOP and eventually, to glaucoma (the result of elevated IOP, resulting in damage to the nerve connecting our eyes with our brain). Losing that connection will result in permanent lose of vision (& ultimately to blindness).
I’ve blogged on the connection between dry eyes and glaucoma medications, so it should be obvious that patients on glaucoma medications are more prone to dry eye. What is also true, is that approximately 1 out of 10 average people placed on steroid eye drops will eventually (within weeks to months) have elevated IOP related to the steroids (the so-called “steroid responders”). Those with a tendency towards glaucoma (strong family history, and/or a tendency towards elevated IOPs and/or with “susceptible appearing nerves”), will have a likelihood of being a steroid responder as much as 1 out of 2 times. This means it is critical to monitor IOP when patients are being carried on topical steroids – to determine if they are a “steroid responder” and may progress to getting glaucoma. It is important to recognize that IOP is a relative number – and that some eyes may progress to severe glaucoma with IOP numbers that might be “normal” for others – where some patients may appear relatively immune to pressures that might normally cause glaucoma for others – so it is important to work closely with your eye doctors to determine what IOP is good for you.
More tests and interpretations coming next week!
Is it safe to buy an eye drop? “FDA issues warning letters to 8 companies for marketing unapproved eye products”
The recent news about people losing vision, eyes, and even lives from contaminated artificial tears already seems enough to convince us that “all eye drops are suspect.” This week’s FDA warning about 8 companies marketing “unapproved” eye products only heightens these concerns. Or does it? The good news is that - to my knowledge, no untowards injuries have been attributed to these products as yet. More good news is that the FDA is “on guard.,” as they should be - to protect us consumers from companies that don’t follow their rules (and their rules are strict for a good reason).
As most of you who follow my posts would know, my practice is devoted to keeping people safe - and helping them help keep their eyes in tip top shape. This means the bulk of what I do is to help my patients make more and better tears while ensuring the health of their ocular surface. In a perfect world, there would be no need for “artificial tears” (or related products) as everyone would have perfect tears. So my practice shyes from recommending artificial tears, as they can mask symptoms and allow patients who could make adequate tears if they worked at it. That “kicking the can down the road” without dealing with root causes, encourages the tear-making apparatus to stall and then to whither and go dry. Keeping that apparatus in good shape takes work - kind of like keeping teeth in good shape. And while we all appreciate eating, we tend to take vision for granted.
It is important to acknowledge that some - despite best efforts and for a variety of reasons beyond their control, simply cannot make a healthy tear in sufficient quantities, to keep the surface of their eyes healthy. And in today’s hard driving world of staring at screens all day, even the best tear producers may need a little help now and again. I therefore do recommend an “as needed” use of artificial tears and related products when it is necessary - but continue to push my patients (and readers) to work on making their best tears. My hat is off to the FDA and all of the people involved in keeping companies on track providing safe, effective products crucial to our health. The short story about these companies is here (and the full story from the FDA is in a link below that): From Healio:(https://www.healio.com/news/optometry/20230914/fda-issues-warning-letters-to-8-companies-for-marketing-unapproved-eye-products?utm_source=selligent&utm_medium=email&utm_campaign=news )
“September 14, 2023
1 min read
FDA issues warning letters to 8 companies for marketing unapproved eye products
The FDA has issued warning letters to eight companies for manufacturing or marketing unapproved ophthalmic drug products, the agency announced in a press release.
In an effort to protect U.S. consumers from potentially harmful eye products, the FDA addressed those that have been illegally marketed to treat conditions such as conjunctivitis, cataracts and glaucoma. Some of the warning letters also cited quality issues related to product sterility.
Eight companies received letters from the FDA that warn of legal action should they fail to correct violations for manufacturing and marketing unapproved ophthalmic products. Image: Adobe Stock.
The companies that received warning letters are Boiron, CVS Health, DR Vitamin Solutions, Natural Ophthalmics, OcluMed, Similasan AG/Similasan USA, TRP Company and Walgreens Boots Alliance.
“The FDA is committed to ensuring the medicines Americans take are safe, effective and of high quality,” Jill Furman, director of the Office of Compliance for the FDA’s Center for Drug Evaluation and Research, said in the release. “When we identify illegally marketed, unapproved drugs and lapses in drug quality that pose potential risks, the FDA works to notify the companies involved of the violations.”
The FDA requested that the companies respond within 15 days of receiving the letters and include a plan to correct the violations. Should the companies fail to comply, the FDA plans to pursue legal action, which may include product seizure and a court order to stop the manufacturing and distribution of an unapproved product. Some companies were also placed on import alert to keep their products from entering the U.S.
“We will continue to investigate potentially harmful eye products and work to ensure violative products stay off store shelves so that consumers can continue taking the medicines they need without concern,” Furman said in the release.”
The FDA link here for those who want the deeper dive:
Stay safe!
Can (CCH) Conjunctivochalasis (or anything to do with poor health) get better without surgery?
Maybe the better question is: How does our body repair itself and how can we assist it in that process?
General Wisdom is that our body turns over much of itself every 7-10 years. Corneal epithelium turns over every 2 weeks.
So it makes sense that outwardly irregular surfaces (or any disease state) can improve over time - assuming we take away the issues that drove it to “go bad” in the first place. I have seen degrees of improvement in CCH without surgery - the key is to start making enough quantity and quality of tears. With great tears, most symptoms of CCH improve (we see some patients with relatively severe CCH that have few if any related signs or symptoms). With poor tears, even mild to moderate degrees of CCH can become problematic and will tend to progress over time. This relates to the fact that plenty of good tears can wash easily over the eye with every blink - even with lots of pleats, folds and wrinkles in the conjunctiva (CCH). But with poor tears, those wrinkles really get in the way of the tears. Equally, if not more significant, the “gutter” or “reservoir” below the lower lid that is bordered by the eyeball, is shortened by the folds, so it can hold fewer tears.
My general push is to try every avenue that helps my patients make more and better tears before “fixing” the CCH (usually with the plications I’ve blogged on and published in my study). For more on CCH, see these earlier posts: https://www.eyethera.com/blog/what-is-conjunctival-chalasis-cch-and-why-should-i-care and for some embedded links to see how I actually do my treatments (and a study I published on the success of these treatments), see:
https://www.eyethera.com/blog/conjunctival-chalasis-cch-part-2-how-do-we-fix-it
Lastly:
https://www.eyethera.com/blog/cch-part-3-when-do-we-treat-cch-and-what-are-the-options
Healthy tears are also critical to healing the surface of the eye - so if, after working hard to improve the amount and quality of tears, the total volume is still suboptimal, then it often makes sense to fix the CCH, so that what a patient has for a tear, can better do its job.
Much research is being aimed at finding better ways to heal the surface when the tears are not up to the job. If the nerves are damaged (common in dry eye disease), then healing the nerves may be needed first. My earlier post on healing a “broken” surface of the eye is found here: https://www.eyethera.com/blog/what-to-do-when-the-surface-of-your-eye-gets-broken-scratched-operated-on-infected-or-otherwise-damaged A French study is underway to test another source of biologic material (Wharton’s Jelly - the material between the umbilical cord and the amnion) to heal poorly healing corneal surfaces: https://www.ophthalmologytimes.com/view/upcoming-trial-aims-to-measure-effectiveness-of-wharton-s-jelly-eye-drops-in-keratitis-treatment?utm_source=sfmc&utm_medium=email&utm_campaign=09062023_OT_eNL_Dry%20Eye%20house%20ad_CRU%20house%20ad&eKey=ZWphY2NvbWFAYW9sLmNvbQ==
For those interested in how the cells of the human body “turn over” every 7-10 years, I’ll first note the proviso that turnover does not mean we don’t age (seems obvious) - but it is pretty cool to understand the way our bodies work. This article helps explain how this works (or doesn’t work for some cells): https://www.livescience.com/33179-does-human-body-replace-cells-seven-years.html
More infectious eye drops and an FDA warning
The following is an article I’m adding to my series of bad eye drops. MSM is a controversial OTC product as there is a lot of online banter about reversing cataracts and other broad claims that have yet to have any adequate human trials to back up. Worse is when this comes in a contaminated eyedrop capable of possibly causing severe eye infections. Fortunately the FDA is blowing the whistle on this particular problem.
FDA warns against the use of certain illegally marketed methylsulfonylmethane (MSM) eye drops due to contamination
Aug 23, 2023
Martin David Harp
News
Article
The organization says to stop using Dr. Berne’s and LightEyez MSM drops immediately due to bacterial contamination, fungal contamination, or both.
(Image Credit: AdobeStock/Regina)
(Image Credit: AdobeStock/Regina)
The US Food and Drug Administration (FDA) is warning consumers to cease use and not purchase Dr. Berne’s MSM Drops 5% Solution and LightEyez MSM Eye Drops – Eye Repair due to bacterial contamination, fungal contamination, or both.
According to the FDA,1 using contaminated eye drops could result in a minor to serious vision-threatening infection which could possibly progress to a life-threatening infection.
While the FDA states they are unaware of any adverse event reports associated with the use of either product, patients who have signs or symptoms of eye infection after use should consult their health care professional immediately.
The Dr. Berne’s and LightEyez eye drop products contain methylsulfonylmethane (MSM) as an active ingredient. According to the FDA, these products are unapproved drugs and illegally marketed in the US. There are no legally marketed ophthalmic drugs that contain MSM as an active ingredient in the US.1
The FDA conducted sampling and testing based on the products’ intended use in the eyes, as well as because of the recent uptick in manufacturing issues with eye drops. According to the FDA, testing showed the products were contaminated with microbes and were not sterile.
Furthermore, the FDA identified bacillus bacterial contamination and exophiala fungal contamination in Dr. Berne’s MSM Drops. While the LightEyez MSM Eye Drops showed bacterial contamination from pseudomonas, mycobacterium, mycolicibacterium, and methylorubrum.1
According to the FDA, Dr. Berne agreed to a voluntary recall of their eye drops on August 21, 2023. While LightEyez Limited has not responded to the FDA’s request for a discussion over the concerns and has taken no action regarding a recall.1
References:
FDA warns consumers not to purchase or use certain methylsulfonylmethane (MSM) eye drops due to contamination. FDA. Press Release. August 22, 2023. Accessed August 23, 2023.https://www.fda.gov/drugs/drug-safety-and-availability/fda-warns-consumers-not-purchase-or-use-certain-methylsulfonylmethane-msm-eye-drops
This article comes from: https://www.ophthalmologytimes.com/view/fda-warns-against-the-use-of-certain-illegally-marketed-methylsulfonylmethane-msm-eye-drops-due-to-contamination?utm_source=sfmc&utm_medium=email&utm_campaign=08262023_OT_OYS-23-OPD0522_NOV-23-OPD0533_eNL_Oyster%20Point%20Dry%20Eye%20TRC_Novartis%20Viewpoints&eKey=ZWphY2NvbWFAYW9sLmNvbQ==